surgerymaxxingsoon

Mistral
- Joined
- Oct 22, 2025
- Posts
- 2,230
- Reputation
- 6,248
Thread Song:
Disclaimer:
This information is for educational purposes only.
 Will my surgery be approved?
Will my surgery be approved?
Disclaimer:
This information is for educational purposes only.
 Will my surgery be approved?
Will my surgery be approved?• First off, you need to have insurance. I won’t get into detail on obtaining insurance, but hopefully you have an option either through your employer or healthcare.gov. I believe if you are under age 26, you can still be on your parents plan, so you may want to look into switching to theirs for the purpose of this surgery if they have a better plan (just be sure to offer to pay for your portion of the premiums, as their costs will go up). If you are in the process of choosing insurance during an open enrollment period, you can factor each plan’s coverage of jaw surgery into your decision. Additionally, as most of us are healthy young people with limited funds, you may have been opting for a low premium, high deductible plan you should do the math on whether it’s more cost effective to opt for a higher premium plan if you know you are having surgery in the next year.
 What Insurance Cares About: “Medical Necessity”
What Insurance Cares About: “Medical Necessity”• You are looking to find out under what circumstances your insurance plan deems jaw surgery “medically necessary”. “Medically necessary” means your insurance thinks you have a big enough health problem that they will pay to have it corrected. Maybe you think you have a large overbite, but your insurance might say it needs to be one millimeter larger before they will pay for it.
 Find Your Plan’s Orthognathic Surgery Policy
Find Your Plan’s Orthognathic Surgery Policy
 Find Your Plan’s Orthognathic Surgery Policy
Find Your Plan’s Orthognathic Surgery Policy• You can look into this before ever seeing an orthodontist or surgeon by looking up the medical policy document for orthognathic surgery with your insurance plan - it may be called something else such as clinical guidelines. The policy document will go into detail about exactly what scenarios surgery is covered. All you have to do is read through it and see if your own case fits one of their scenarios.
Example:https://www.anthem.com/medpolicies/abcbs/active/gl_pw_d083869.html
You may be able to search for the document on their website, but you may have to call and ask for it. They shouldn’t fight you on providing it.
• As you are researching for insurance purposes, all types of jaw surgery are broadly deemed “orthognathic surgery”. If you are speaking to a representative, “jaw surgery” will do just fine, but if you are reading through documents, you’ll want to be looking for the term “orthognathic”.
 What You’re Looking For
What You’re Looking For• Be aware that there may be more than one medical policy document pertinent to your situation. Anthem for example has one broadly for orthognathic surgery which mostly speaks to malocclusion and other standard jaw measurements, and then separate documents for sleep apnea and TMJ treatments.
• This is where it’s helpful to have an appointment with ortho or at least dentist, who can take a CBCT or x-ray to obtain your measurements. I did a rough, preliminary ceph analysis myself, all you need is a rule and protractor. Or you may have issues so large, they are obviously outside of the stated norms, no imaging necessary (for your investigative purposes anyway, down the line it definitely will be).
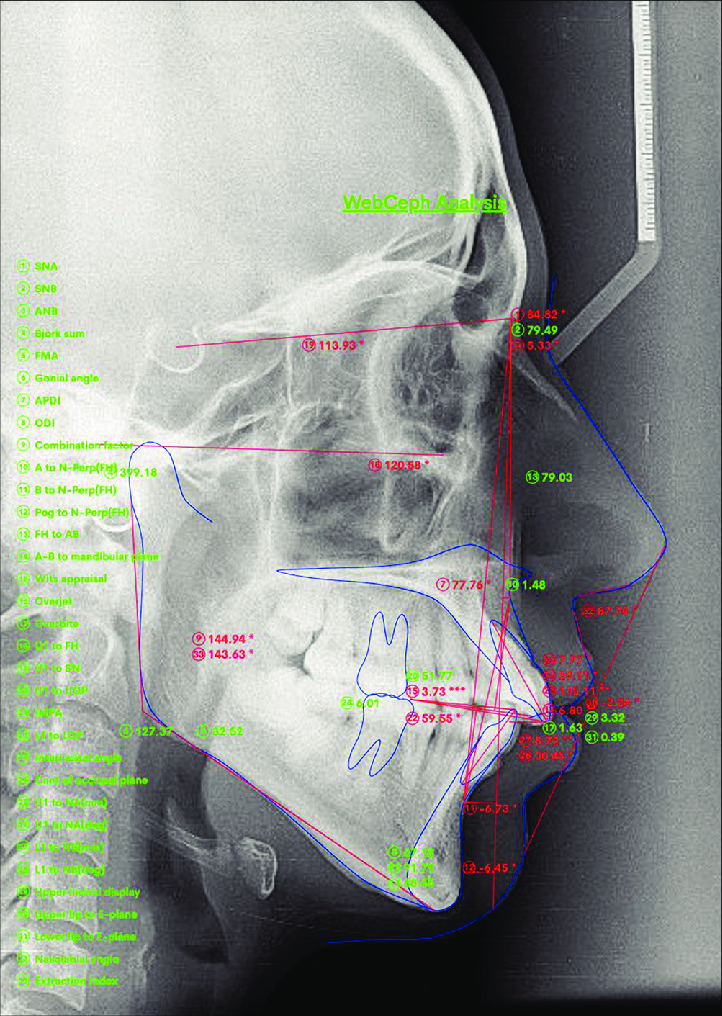
Lateral Cephalogram Showing WEBCEPH
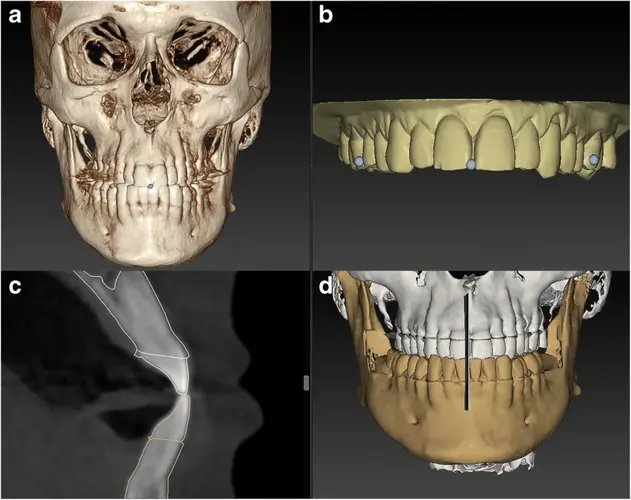
CBCT Scan

Dental Imaging X-Ray's
 Important: There May Be Multiple Policies
Important: There May Be Multiple Policies• If you are pursuing jaw surgery for known or suspected sleep problems, consider a WatchPAT sleep test, available online for about $200, which is far cheaper than my hospital-provided home sleep study. This measures both AHI and RDI and should suffice for insurance approval.
• If you find that your situation IS NOT COVERED under these documents, you’re in for a hard battle. You will definitely need a supportive surgeon to fight for your case, and it may be best to look into switching insurance companies for one that offers more favorable coverage, if possible.
• If you found that your scenario should be covered, you now have ammo to speak to providers and insurance about why you want the surgery. If you’re shy about speaking up for yourself and your needs, and you may be seeing doctors who are originally dismissive of your problems it’s over (not completely).
• The reality is most oral surgeons only do jaw surgeries for large overbites or underbites. Anything else and they’re going to be surprised to see you, especially if you’re referring yourself (i.e. not seeing them on an orthodontist or dentist’s recommendation).
 Pre‑Approval & Appeals
Pre‑Approval & Appeals• Once you have a surgeon, their office is going to be the one submitting the insurance claims for you, 99% of the time. They will submit a pre-approval request before the surgery takes place. If you are not approved on the first request, but know you should be based on your insurance’s own document, you can feel confident in disputing their decision.
 Okay, It’s Medically Necessary — What Will I Pay?
Okay, It’s Medically Necessary — What Will I Pay?• In Network Surgeon: The best case scenario is if you will be using an in-network surgeon at an in-network hospital or facility. You can look for your “max out of pocket” amount on your insurance plan, and boom, that’s it. That’s all you will pay for the surgery and any in-network medical appointments that happen in the same year as the surgery. (Insurance rolls over at the start of each calendar year and you “start fresh” toward your deductible and max out of pocket amounts.)
Notes: Keep in mind, orthodontics are likely to be a separate, additional amount depending on how nice of an insurance plan you have.
Notes: It is exceedingly rare you will pay less than your max out of pocket amount, because jaw surgery is just really expensive.
• I usually see max out of pocket amounts range anywhere from $3k to $15k. If you know your surgeon is in-network for a certain insurance company, this is a really compelling reason to choose a plan with them with a low max out of pocket, regardless of premiums or deductibles.
• As you are searching for a surgeon, MAKE SURE they are in your medical network. It’s confusing because many will be in your dental network. Jaw surgery is billed through the medical network, so that’s the one you’re looking for.
 Out‑of‑Network (OON) Surgeon — Read Carefully
Out‑of‑Network (OON) Surgeon — Read Carefully• You might notice that your plan has an “out of network maximum out of pocket” amount that is either the same or different from the in-network max.
 DO NOT LET THIS FOOL YOU
DO NOT LET THIS FOOL YOU into thinking that number is all you will pay for an out-of-network surgeon.
into thinking that number is all you will pay for an out-of-network surgeon. The Trap
The Trap• Insurance companies have a contracted rate with their in-network providers that both parties agree to. If you work with an OON provider, insurance is still only going to pay an amount similar to their contracted rates, but the provider, being out of network, can charge whatever their little heart desires. Whatever the difference is between those two amounts is what you will be stuck with - this is called “balance billing”, and where you hear horror stories of people getting stuck with abhorrent amounts of medical debt.
• So how do you know how much your insurance will pay towards an out-of-network surgeon? You will want to call your insurance and ask for the “maximum allowed amount” for an OON provider for the specific procedures you’ll be going through. It’s easy to get this term confused with “max out of pocket amount”, but this is not the amount you pay, it’s the max amount the insurance contributes.
 What to Ask Insurance (Exact Wording Matters)
What to Ask Insurance (Exact Wording Matters)• They may make you jump through some hoops, but you are entitled to this information. You will be asked to provide surgical codes for each procedure (it’s not just “jaw surgery”, there will be separate codes for lefort 1, genioplasty, etc.) that your surgeon should be able to give you. If not, at least get the names for each separate procedure and then call your insurance and ask for the associated codes, or they should be listed on the medical policy documents we discussed above. You will probably also need surgeon and facility information, but if there are any details you don’t know, just tell them and they can probably look it up themselves.
 Lock Costs In Before Surgery
Lock Costs In Before Surgery• Once you have the max allowed amounts, you can relay this info to your provider, who can then create a more informed quote for you. If they are experienced with dealing with insurance, they likely already have a good idea on what the amounts will be; still, it’s a good idea to do your research and make sure everybody is on the same page.
• You should be able to come to an agreed amount with your provider before the surgery takes place. It is crazy the way that insurance will only offer up the amount you pay after the procedure takes place, but you don’t need to settle for this. Make sure the costs are agreed to and signed off on with your provider up-front, everything from surgeon’s fee, anesthesia, and hospital or facility fees.
• It does not hurt to try to negotiate on fees; the worst they can do is say no, and you may save yourself thousands of dollars. Be sure to read through everyyything on a payment contract before signing it.
• If your OON provider's office is not willing to work with you on this agreement pre-surgery and just wants to leave you to the mercy of insurance... you will almost certainly be stuck with a massive bill. I'd HIGHLY suggest finding a different surgeon.
 Why Claims Look Scarier Than What You Pay
Why Claims Look Scarier Than What You Pay• Note: that the amount you are asked to pay will probably be lower than what you will eventually see on the insurance claim; don’t panic, that’s a good thing. The provider bills the insurance company a huuuge amount in order to squeeze the largest reimbursement out of them. Then they have a separate, more reasonable charge that goes to you. Again, just make sure that charge is agreed to up front.
 No In‑Network Option? Request Gap Coverage
No In‑Network Option? Request Gap Coverage• Out of network is too expensive for me, but it’s the only option. Is there anything I can do? Yes. You can request a “gap coverage request” which my insurance calls an “in for out” request. This means that they will cover the provider as though they are in-network based on the fact that there is something lacking (aka the “gap”) in their coverage plan. You will call your insurance and let them know that you have a medically necessary procedure with no option for an in-network provider. They will start the request for you after you provide the same procedural, surgeon, and facility info mentioned above. You will also need to have your provider send in their diagnostic and treatment plan for you, or have it on hand to fax yourself. Your provider and surgeon may be able to work out this request between themselves.
• You’ll want to make this request with plenty of time before surgery as it takes about a month to get a decision back.
• Keep in mind you may have a facility, surgeon, anesthetist, etc, who are each out of network and would require their own individual request.
 Surgeons Who Don’t Take Insurance
Surgeons Who Don’t Take Insurance• Surgeon who do not accept insurance: If your surgeon is not just OON, but doesn't take insurance at all, then the sky’s the limit. They may charge an absolutely exorbitant amount, and you will get nothing back from your insurance. But they also have the most flexibility. That means you can negotiate with them -- if they say surgery will be $75k, say that’s not feasible for and ask if they can come down to $xx. Hopefully you can meet in the middle. You can consider asking them for patient referrals, and then you can ask those patients what they paid to get a sense of the range in amounts and flexibility the provider has.
Last edited:


 good thread aswell
good thread aswell