7evenvox22
.
- Joined
- May 29, 2025
- Posts
- 599
- Reputation
- 1,495
Introduction
Testosterone (T), the primary endogenous sex hormone in men, is a bioidentical anabolic-androgenic steroid (AAS) essential for male physiology. Many people think of testosterone as the boring default androgen that has no interesting properties apart from agonizing the androgen receptor, but this is not true. Testosterone does have some unique properties that deviate it from being purely an androgen receptor agonist.WISP-2 mRNA expression
Testosterone promotes muscle growth and fat loss by increasing WISP-2 mRNA expression (likely due to its aromatization into estradiol), which regulates growth factors like IGF-1 and TGF-β. WISP-2 enhances lean mass, reduces fat, and improves insulin sensitivity. [1]
Insulin sensitivity
Testosterone increases insulin sensitivity primarily through its metabolism into estradiol and DHT. It decreases glucocorticoids (cortisol) in the liver through 5a-reductase, which decreases catabolism and increases insulin sensitivity. It also greatly increases glucose metabolism through its aromatization into estradiol and subsequent agonism of ER-a.
References
[1] https://pmc.ncbi.nlm.nih.gov/articles/PMC8396102/
Introduction
Oxandrolone, also known as Anavar, is an androgen known for its strong anabolic effects with minimal androgenic activity. It effectively increases bone density and height velocity, reduces abdominal fat, enhances strength, and counters catabolism but negatively impacts lipids. Despite being labeled as a "women’s drug," it is potent for fat loss and muscle preservation in men as well.
Increased Height Velocity
Oxandrolone has been used clinically to promote growth in children with growth disorders (e.g., Turner syndrome, constitutional delay of growth and puberty). Unlike testosterone, which accelerates bone maturation and can prematurely close growth plates (epiphyseal fusion), oxandrolone appears to increase height velocity with less advancement in bone age, making it a useful therapeutic option.
The mechanisms for this are:
Oxandrolone uniquely reduces subcutaneous and visceral fat more effectively than testosterone or nandrolone. This is linked to its stimulation of hepatic ketogenesis, which enhances fat oxidation. However, this benefit comes with a tradeoff: worsened lipid profiles: oxandrolone increases hepatic lipase activity, shifting HDL to smaller, atherogenic VLDL particles, raising cardiovascular risk. Since it doesn’t aromatize, it lacks estrogen’s protective lipid effects, exacerbating this issue. By boosting fatty acid oxidation, oxandrolone promotes fat loss but also increases ketogenesis, which spares protein while worsening lipid metabolism.
Anti-Catabolism
Oxandrolone modulates glucocorticoid receptors (GR) via androgen receptor (AR) crosstalk, reducing cortisol’s catabolic effects. This mechanism differs from other AAS, offering potential synergy in steroid stacks.
Strength Benefits
Oxandrolone rapidly enhances strength, partially by increasing creatine synthesis and phosphocreatine stores, supporting anaerobic performance. This effect is notable given its low androgenic potency.
Conclusion
Oxandrolone excels at fat loss, anticatabolism, and strength gains but significantly harms lipids. Its benefits—enhanced ketogenesis, cortisol modulation, and creatine synthesis—must be weighed against cardiovascular risks.
Oxandrolone, also known as Anavar, is an androgen known for its strong anabolic effects with minimal androgenic activity. It effectively increases bone density and height velocity, reduces abdominal fat, enhances strength, and counters catabolism but negatively impacts lipids. Despite being labeled as a "women’s drug," it is potent for fat loss and muscle preservation in men as well.
Increased Height Velocity
Oxandrolone has been used clinically to promote growth in children with growth disorders (e.g., Turner syndrome, constitutional delay of growth and puberty). Unlike testosterone, which accelerates bone maturation and can prematurely close growth plates (epiphyseal fusion), oxandrolone appears to increase height velocity with less advancement in bone age, making it a useful therapeutic option.
The mechanisms for this are:
- - Oxandrolone increases insulin-like growth factor 1 (IGF-1) production, a key mediator of longitudinal bone growth.
- - Studies show it enhances pulsatile GH secretion, further supporting growth.
- - It greatly enhances collagen synthesis, and improves bone density more than any other androgen.
- - Unlike testosterone (which converts to estrogen via aromatase, accelerating growth plate closure), oxandrolone does not aromatize.
- - Its weak androgenic activity means it stimulates growth without rapidly advancing bone age, allowing for a longer growth window.
- - By modulating glucocorticoid receptor (GR) activity, oxandrolone reduces cortisol’s catabolic effects on bone and muscle, preserving growth potential.
Oxandrolone uniquely reduces subcutaneous and visceral fat more effectively than testosterone or nandrolone. This is linked to its stimulation of hepatic ketogenesis, which enhances fat oxidation. However, this benefit comes with a tradeoff: worsened lipid profiles: oxandrolone increases hepatic lipase activity, shifting HDL to smaller, atherogenic VLDL particles, raising cardiovascular risk. Since it doesn’t aromatize, it lacks estrogen’s protective lipid effects, exacerbating this issue. By boosting fatty acid oxidation, oxandrolone promotes fat loss but also increases ketogenesis, which spares protein while worsening lipid metabolism.
Anti-Catabolism
Oxandrolone modulates glucocorticoid receptors (GR) via androgen receptor (AR) crosstalk, reducing cortisol’s catabolic effects. This mechanism differs from other AAS, offering potential synergy in steroid stacks.
Strength Benefits
Oxandrolone rapidly enhances strength, partially by increasing creatine synthesis and phosphocreatine stores, supporting anaerobic performance. This effect is notable given its low androgenic potency.
Conclusion
Oxandrolone excels at fat loss, anticatabolism, and strength gains but significantly harms lipids. Its benefits—enhanced ketogenesis, cortisol modulation, and creatine synthesis—must be weighed against cardiovascular risks.
Growth Hormone (GH) and IGF-1: Their Critical Role in Bone Development
Introduction
Growth hormone (GH) and insulin-like growth factor-1 (IGF-1) are central regulators of skeletal growth, bone density, and metabolism. GH, secreted by the pituitary gland, stimulates IGF-1 production primarily in the liver, creating the GH-IGF-1 axis, which governs bone formation, mineralization, and remodeling. This article explores how GH and IGF-1 influence bone development and what happens when their signaling is disrupted.1. The GH-IGF-1 Axis and Bone Biology
A. Growth Hormone (GH) – The Primary Stimulator
- Source: Pituitary gland (regulated by GHRH and inhibited by somatostatin).
- Direct Effects on Bone:
- Stimulates chondrocyte proliferation in the growth plate, enabling longitudinal bone growth.
- Enhances osteoblast activity (bone-forming cells).
- Indirect Effects via IGF-1:
- GH triggers hepatic IGF-1 secretion, which mediates most of its growth-promoting effects.
B. IGF-1 – The Key Mediator
- Source: Primarily liver (endocrine IGF-1), but also produced locally in bone (paracrine/autocrine effects).
- Effects on Bone Cells:
- Osteoblasts: Promotes differentiation, collagen synthesis, and mineralization.
- Chondrocytes: Supports cartilage growth at the epiphyseal plate.
- Osteoclasts: Modulates bone resorption indirectly via RANKL/OPG balance.
2. How GH and IGF-1 Drive Bone Development
A. Fetal and Childhood Growth
- Prenatal Bone Formation: IGF-1 (more than GH) is crucial for early skeletal development.
- Postnatal Growth:
- GH and IGF-1 drive endochondral ossification (longitudinal growth via growth plate expansion).
- Deficiency in either hormone leads to short stature (e.g., growth hormone deficiency, Laron syndrome).
B. Adolescence – Peak Bone Mass Acquisition
- Puberty triggers a GH/IGF-1 surge, accelerating bone growth.
- IGF-1 increases bone mineral density (BMD) by enhancing osteoblast activity.
C. Adulthood – Bone Remodeling and Maintenance
- GH and IGF-1 help maintain bone turnover balance (formation vs. resorption).
- Declining GH/IGF-1 with age contributes to osteoporosis.
3. Disorders of GH-IGF-1 Signaling and Bone Health
A. GH Deficiency (GHD)
- In Children: Short stature, delayed bone age, reduced BMD.
- In Adults: Increased fracture risk, low bone turnover.
- Treatment: GH replacement therapy improves bone mass.
B. GH Excess (Acromegaly)
- Effects:
- Excessive growth plate stimulation → enlarged bones (jaw, hands, feet).
- Disorganized bone structure → increased fracture risk despite high BMD.
- Treatment: Surgery, somatostatin analogs, or GH receptor antagonists.
C. IGF-1 Deficiency (Laron Syndrome)
- Cause: GH receptor mutation → low IGF-1 despite high GH.
- Effects: Severe short stature, osteopenia.
- Treatment: Recombinant IGF-1 therapy.
D. Age-Related Decline (Somatopause)
- Reduced GH/IGF-1 contributes to senile osteoporosis.
- Potential therapies: GH/IGF-1 supplementation (controversial due to cancer risks).
4. Clinical and Therapeutic Implications
A. GH Therapy in Growth Disorders
- Used in pediatric GHD, Turner syndrome, and chronic kidney disease.
- Improves height and bone mineralization.
B. IGF-1 Therapy (e.g., Mecasermin)
- Approved for severe primary IGF-1 deficiency.
- Enhances bone growth but requires careful monitoring (risk of hypoglycemia).
C. Risks of Overstimulation
- Acromegaly: Uncontrolled bone overgrowth.
- Cancer Concerns: Elevated IGF-1 may promote tumor growth (e.g., prostate, breast cancer).
Practical Application
Example stack for maximizing bone growth via GH and IGF-1:- - 5iu growth hormone per day
- - 25mg MK677 per day
Introduction to PTH analogs
Parathyroid hormone (PTH) analogs are synthetic derivatives of the endogenous PTH peptide, which plays a critical role in calcium and phosphate homeostasis. These analogs are primarily used in the treatment of osteoporosis and hypoparathyroidism. Unlike antiresorptive agents (e.g., bisphosphonates), PTH analogs stimulate bone formation, making them unique anabolic therapies.Physiology of Parathyroid Hormone
PTH is an 84-amino acid peptide secreted by the parathyroid glands in response to low serum calcium levels. Its key functions include:- Bone remodeling: PTH enhances osteoclast activity (indirectly via RANKL) and osteoblast differentiation, leading to both bone resorption and formation.
- Renal calcium reabsorption: PTH increases calcium reabsorption in the distal tubules while promoting phosphate excretion.
- Vitamin D activation: PTH stimulates renal 1α-hydroxylase, converting 25-hydroxyvitamin D to active 1,25-dihydroxyvitamin D (calcitriol), enhancing intestinal calcium absorption.
- Continuous high levels (as in hyperparathyroidism) lead to net bone loss.
- Intermittent low doses (mimicking physiological pulses) promote bone formation.
PTH Analogs: Mechanism of Action
PTH analogs are engineered to replicate the anabolic effects of endogenous PTH while minimizing undesirable catabolic effects. The two main FDA-approved analogs are:1. Teriparatide (PTH 1-34)
- Structure: Recombinant fragment containing the first 34 amino acids of PTH (the active binding region).
- Mechanism:
- Binds to PTH1 receptors on osteoblasts, activating cAMP/PKA and Wnt/β-catenin pathways.
- Stimulates osteoblast proliferation and differentiation, increasing bone mineral density (BMD).
- Half-life: ~1 hour (subcutaneous administration).
2. Abaloparatide (PTHrP Analog)
- Structure: Synthetic analog of parathyroid hormone-related protein (PTHrP), sharing homology with PTH.
- Mechanism:
- Selective binding to the RG conformation of PTH1R, favoring bone formation over resorption.
- Shorter receptor activation time compared to teriparatide, reducing hypercalcemia risk.
- Half-life: ~1.7 hours (subcutaneous administration).
Clinical Applications
1. Osteoporosis Treatment
- Indications:
- Postmenopausal women and men at high fracture risk.
- Patients unresponsive to bisphosphonates or with severe osteoporosis (T-score ≤ -3.0).
- Efficacy:
- Teriparatide increases lumbar spine BMD by 9-13% over 18 months.
- Abaloparatide shows similar efficacy with a lower hypercalcemia risk.
- Duration: Limited to 24 months (lifetime) due to osteosarcoma risk (observed in rodent studies).
2. Hypoparathyroidism
- PTH (1-84) (Natpara):
- Full-length recombinant PTH for chronic hypoparathyroidism.
- Restores calcium homeostasis, reducing reliance on high-dose calcium and vitamin D.
- Discontinued in 2019 due to manufacturing issues but remains available in some regions.
Pharmacokinetics and Administration
- Route: Subcutaneous injection (daily for teriparatide/abaloparatide).
- Absorption: Rapid, peak concentrations within 30-60 minutes.
- Metabolism: Cleared via renal and hepatic pathways.
Adverse Effects and Contraindications
Common Side Effects
- Hypercalcemia (more frequent with teriparatide).
- Orthostatic hypotension, dizziness.
- Injection site reactions.
Serious Risks
- Osteosarcoma: Seen in preclinical studies (no confirmed human cases, but caution advised).
- Hypercalciuria and nephrolithiasis.
Contraindications
- Paget’s disease of bone.
- Prior radiation therapy to bone.
- Pediatric patients (open epiphyses).
Practical Application
Teriparatide: Administer once per day at 20 micrograms.Abaloparatide: Administer once per day at 80 micrograms.
You can make the decision to slowly titrate the doses up if the doses are well tolerated, but the safety of doing so has not been proven in the literature.
Introduction
Histone deacetylases (HDACs) regulate gene expression by removing acetyl groups from histones, leading to chromatin compaction and transcriptional repression. HDAC inhibitors (HDACi) reverse this process, promoting gene activation. Emerging research highlights their role in modulating androgen receptor (AR) signaling and bone development, particularly when combined with androgen-boosting therapies or osteoblast-stimulating agents. HDAC inhibitors modulate the epigenetic landscape, often amplifying the transcriptional effects of active signaling pathways. When combined with a ligand (e.g., androgens, BMPs), they can enhance downstream gene expression by stabilizing receptors or transcription factors and increasing chromatin accessibility at target genes.HDAC Inhibition and Epigenetic Regulation
1. Chromatin Remodeling & Gene Reactivation
- HDAC inhibition increases histone acetylation, loosening chromatin and reactivating silenced genes.
- This can enhance AR transcriptional activity by making AR-binding sites more accessible.
2. Non-Histone Targets: Androgen Receptors & Bone Proteins
HDACs also deacetylate non-histone proteins, including:- Androgen receptors (AR) – Acetylation stabilizes AR and enhances its transcriptional activity.
- Runx2 – A master regulator of osteoblast differentiation; acetylation promotes bone formation.
- β-catenin – A key Wnt signaling component that stimulates osteogenesis.
HDAC Inhibition & Androgen Receptor Signaling
1. Enhanced AR Sensitivity
- HDAC inhibition increases AR acetylation, preventing its degradation and boosting transcriptional activity.
- In prostate cancer, HDACi like vorinostat synergize with androgen deprivation therapy (ADT) by resensitizing AR to low androgen levels. This is a testament to the efficacy to which HDACi can amplify the transcriptional effects of active signaling pathways.
2. Combined with Androgen Boosters (e.g., SARMs, Testosterone)
- SARMs (Selective Androgen Receptor Modulators) and testosterone upregulate AR signaling.
- Adding HDACi can further amplify AR-driven anabolism in muscle and bone by preventing AR degradation.
HDAC Inhibition & Bone Development
1. Stimulating Osteoblast Differentiation
- HDACi promote Runx2 acetylation, enhancing osteoblast maturation.
- Combined with bone morphogenetic proteins (BMPs) or PTH analogs, HDACi may accelerate bone formation.
2. Synergy with Anabolic Bone Agents
- Teriparatide (PTH1-34) – Increases osteoblast activity; HDACi prolongs its effects.
- Wnt agonists (e.g., Sclerostin inhibitors) – HDACi stabilize β-catenin, further boosting bone growth.
2. IGF-1 Synergy
- IGF-1 stimulates osteoblast proliferation; HDACi enhance IGF-1 receptor signaling by increasing chromatin accessibility at growth-related genes.
- Potential for Fracture Healing: Preclinical studies show HDACi (e.g., sodium butyrate) improve callus formation.
3. Anti-Resorptive Effects
- Some HDACi (e.g., entinostat) suppress osteoclastogenesis, protecting bone mass.
Therapeutic Applications
1. Muscle-Bone Crosstalk
- Combining SARMs + HDACi + IGF-1: Could simultaneously enhance lean mass and bone density in sarcopenia/osteoporosis.
- Myostatin Inhibition + HDACi: May further amplify muscle growth.
Height Growth
1. Epiphyseal Plate Modulation
- Growth Plate Chondrocytes: HDAC inhibition promotes SOX9 and Runx2 acetylation, enhancing chondrocyte proliferation and differentiation.
- IGF-1 Synergy: HDACi increase IGF-1 sensitivity, expediting the rate of growth before epiphyseal closure.
- Delayed Bone Maturation: Unlike androgens (which accelerate growth plate fusion via estrogen conversion), HDACi extends the growth window by suppressing osteoclast-mediated plate closure.
2. Clinical Implications
- Pediatric Growth Disorders: HDACi (e.g., valproic acid) could complement GH therapy in short stature cases.
- Post-Pubertal Height: Unlikely to increase height after plate fusion, but can improve bone density.
- HDAC Inhibition and Height Growth
Clavicle Growth
1. Clavicular Expansion Mechanisms
- Intramembranous Ossification: The clavicle forms via direct bone deposition (not cartilage). HDACi enhance Runx2 and Osterix activity, stimulating osteoblast differentiation.
- Androgen/IGF-1 Synergy: Testosterone and IGF-1 widen clavicles; HDACi may amplify this effect by increasing AR and IGF-1R sensitivity.
- 2. Potential Applications
- Aesthetic Broadening: Bodybuilders and athletes may see enhanced shoulder width when combining HDACi with androgens.
- Fracture Healing: Accelerated clavicle repair via osteoblast activation.
HDAC Inhibition and Mandibular Growth
1. Condylar Cartilage & Ramus Expansion
- Chondrocyte Proliferation: HDACi promote aggrecan and collagen II expression, improving mandibular condyle growth.
- Androgen-Driven Effects: DHT/AR signaling increases mandibular robustness; HDACi may enhance this via AR acetylation.
- 2. Dental & Orthodontic Implications
- Late-Growth Enhancement: May aid class II malocclusion correction by stimulating condylar growth in adolescents.
- Surgical Adjunct: Could improve outcomes in mandibular distraction osteogenesis.
HDAC Inhibition and Maxillary Growth
1. Sutural Expansion & Forward Projection
- Sutural Osteogenesis: HDACi increase BMP and Wnt signaling, promoting midface advancement.
- PTHrP Interaction: Parathyroid hormone-related peptide regulates maxillary sutures; HDACi may amplify its effects.
- 2. Clinical Potential
- Maxillary Hypoplasia: Could complement facemask therapy in growing patients.
- Cleft Palate Repair: Enhanced bone formation at graft sites.
Combination Strategies for Optimized Growth
1. Androgens + HDACi
- Testosterone: Boosts AR-driven bone growth; HDACi prevent AR degradation.
- Anavar: Increases bone density and height velocity
- Trenbolone: Very high affinity for the androgen receptor; HDACi will be able to amplify these transcriptional effects and further upregulate AR.
- 2. Growth Factors + HDACi
- IGF-1 LR3 / GH: HDACi increase IGF-1R sensitivity, synergizing with GH’s conversion into IGF-1 and other IGF-1 analogues.
- BMP-2/7: Accelerates osteogenesis in targeted areas (e.g., maxilla).
- 3. Mechanical Loading + HDACi
- Orthodontics/Orthopedics: HDACi can enhance bone remodeling in response to functional appliances, palatal expanders.
- Manual mechanical force techniques: the remodeling response to manual techniques that apply mechanical force to bones is also amplified. This will be expanded on in the craniofacial development chapter.
Risks
1. Asymmetry Risk
- Uneven HDACi + mechcanical loading could lead to skewed growth (e.g., mandibular asymmetry). It is important to apply force evenly and constantly reassess the symmetry of growth.
- 2. Overgrowth Concerns
- Uncontrolled osteoblast activation might cause excessive bone thickening (e.g., prognathism). This is not an issue if your face is sufficiently underdeveloped in these areas, but it is important to note if your facial bones are sufficient and you are instead focusing on height and frame development, with craniofacial growth becoming an unwanted side effect.
Introduction to Aromatase Inhibitors
Aromatase inhibitors (AIs) are drugs that block the conversion of androgens (testosterone, androstenedione) into estrogens (estradiol, estrone). While primarily used in breast cancer treatment and sometimes in managing gynecomastia, AIs have gained attention for their potential effects on bone growth—particularly in increasing height, clavicle length, and mandibular/maxillary development. This article explores the mechanisms behind these effects, clinical evidence, and potential applications.The Role of Estrogen in Bone Growth and Epiphyseal Closure
Bone growth is regulated by a complex interplay of hormones, with estrogen playing a crucial role:- Growth Plate Fusion:
- Estrogen accelerates epiphyseal (growth plate) closure in both males and females.
- In males, testosterone is peripherally converted to estrogen via aromatase, which ultimately mediates growth plate closure.
- Studies on males with aromatase deficiency or estrogen resistance show delayed epiphyseal fusion, leading to continued linear growth into adulthood (e.g., cases of men growing beyond age 25).
- Bone Maturation vs. Elongation:
- Estrogen promotes bone mineralization and skeletal maturation.
- By inhibiting estrogen synthesis, AIs may prolong the growth phase, allowing for additional height gain.
Aromatase Inhibition and Increased Height
Mechanism
- Delayed Epiphyseal Closure:
- AIs reduce estrogen levels, slowing growth plate ossification.
- This prolongs the window for longitudinal bone growth.
- Increased IGF-1 Activity:
- Estrogen suppresses growth hormone (GH) and insulin-like growth factor 1 (IGF-1).
- Lower estrogen → higher GH/IGF-1 → enhanced chondrocyte proliferation in growth plates.
Clinical Evidence
- Studies in Adolescent Males:
- A 2009 study (Mauras et al., J Clin Endocrinol Metab) found that letrozole + testosterone in adolescent boys delayed bone age advancement, increasing predicted adult height by ~5 cm compared to testosterone alone.
- Another study (Hero et al., JCEM 2005) showed that anastrozole in boys with short stature increased near-final height by ~6 cm.
- Case Reports:
- Males with aromatase deficiency exhibit continued growth into their 20s with unfused growth plates.
Limitations
- Effectiveness Depends on Growth Plate Status:
- Works best in adolescents with open growth plates.
- Minimal effect in adults after fusion.
- Potential Side Effects:
- Reduced bone mineral density (BMD) due to low estrogen.
- Increased fracture risk if used long-term.
Aromatase Inhibition and Clavicle Growth
Why the Clavicle?
- The clavicle is one of the last bones to fuse (early-to-mid 20s).
- It grows via intramembranous ossification (unlike long bones, which rely on endochondral ossification).
Possible Effects of AIs
- Prolonged Growth Period:
- Since clavicular growth plates remain open longer with estrogen suppression, AIs may allow additional lateral growth.
- Increased Androgen Exposure:
- Testosterone (unopposed by estrogen) may enhance osteoblast activity in membranous bones.
Evidence
- Limited Direct Studies:
- No large-scale trials, but anecdotal reports suggest clavicular widening in late-teens/early 20s males using AIs.
- Bone scans in AI-treated adolescents show delayed sternoclavicular joint fusion.
Aromatase Inhibition and Jaw (Mandible/Maxilla) Growth
Mechanism
- Androgen-Mediated Bone Modeling:
- Testosterone and DHT stimulate osteoblast activity in the mandible and maxilla.
- Without estrogen-mediated inhibition, androgens may enhance jawbone growth.
- Growth Plate-Like Effects in Condylar Cartilage:
- The mandibular condyle has a growth plate-like structure that responds to hormonal signals.
- Estrogen suppression could prolong mandibular growth in adolescents.
Evidence
- Animal Studies:
- Rats treated with AIs show increased mandibular length due to delayed ossification.
- Human Case Observations:
- Males with aromatase deficiency often have more prominent jawlines and broader facial structures.
- Bodybuilders using AIs (often alongside androgens) report enhanced jaw definition, though this may also be due to muscle hypertrophy and fat loss.
Limitations
- Age-Dependent Effects:
- Likely only effective during active growth (puberty to early 20s).
- Minimal impact in adults with fully fused facial bones.
- No Controlled Human Trials:
- Most evidence is indirect or based on androgen-excess conditions.
Potential Applications and Risks
Medical Uses
- Height Augmentation in Adolescents:
- For boys with constitutional delay of growth or idiopathic short stature.
- Often combined with growth hormone therapy.
- Maxillofacial Development:
- Theoretical use in orthodontics for underdeveloped jaws (e.g., retrognathia).
Risks and Side Effects
- Reduced Bone Density: Estrogen is crucial for BMD; long-term AI use may increase osteoporosis risk. It seems prudent to combine heavy aromatase inhibitor usage with PTH analogs.
- Metabolic Effects: Can worsen lipid profiles (increased LDL, decreased HDL).
- Neurotoxicity: Estrogen is important for negating the neurotoxic effects of androgens on the brain. It is important to include neuroprotective compounds, which will be talked about in the upcoming modules.
Practical Application
Exemestane (Aromasin): start with 12.5mg every other dayLetrozole (Femara): start with 0.5mg every other day
Anastrozole (Arimidex): start with 0.5mg every other day
You may titrate up accordingly if you have minimal side effects, but proceed with caution. Crashed estradiol has many harsh symptoms.
Introduction
Transforming growth factor-beta (TGF-β) is a key regulator of bone formation, chondrogenesis, and skeletal remodeling. When combined with HDAC inhibitors (HDACi), androgens, or growth factors (e.g., IGF-1, BMPs), TGF-β agonists may further amplify bone growth in critical areas such as:- Height (long bone elongation)
- Clavicle widening
- Mandibular and maxillary expansion
TGF-β’s Role in Bone Growth
1. Mechanisms of Action
TGF-β signaling influences bone development through:- Stimulation of Mesenchymal Stem Cells (MSCs) → Drives osteoblast and chondrocyte differentiation.
- Enhancement of Extracellular Matrix (ECM) Deposition → Boosts collagen, osteocalcin, and alkaline phosphatase activity.
- Modulation of Growth Plate Chondrocytes → Supports longitudinal bone growth before epiphyseal closure.
2. TGF-β vs. BMP Signaling
While BMPs primarily drive osteoblast differentiation, TGF-β has a broader regulatory role:- Early-stage osteogenesis (MSC recruitment)
- Bone remodeling (coupling osteoblast-osteoclast activity)
- Chondrocyte maintenance (critical for growth plate function)
TGF-β Agonists for Targeted Bone Growth
1. Height Growth (Epiphyseal Plate Stimulation)
- TGF-β1 and TGF-β3 promote chondrocyte proliferation in growth plates.
- Synergy with IGF-1: TGF-β enhances IGF-1 receptor sensitivity, further stimulating long bone elongation.
- HDACi Combo: HDAC inhibition may prolong TGF-β effects by preventing Smad7-mediated suppression of TGF-β signaling.
2. Clavicle Expansion (Intramembranous Ossification)
- TGF-β agonists increase periosteal bone formation, widening clavicles.
- Androgen Combo: Testosterone/SARMs + TGF-β could enhance lateral clavicle growth for broader shoulders.
3. Mandibular & Maxillary Growth
- Mandible: TGF-β stimulates condylar cartilage growth and ramus elongation.
- Maxilla: Enhances sutural expansion (midface projection).
- HDACi Combo: Acetylation of Runx2/Smad4 may amplify osteogenic effects.
Synergistic Strategies: TGF-β + HDACi + Androgens/Growth Factors
1. TGF-β + HDAC Inhibition
- HDACi prevent Smad7 suppression → Prolonged TGF-β/Smad signaling.
- Increased BMP-2 expression → Further osteoblast stimulation.
2. TGF-β + Androgens (Testosterone/DHT/SARMs)
- Androgens upregulate TGF-β receptors in osteoblasts.
- Enhanced mandibular and clavicular growth in androgen-sensitive areas.
3. TGF-β + IGF-1/BMPs
- IGF-1 boosts chondrocyte proliferation, while TGF-β maintains cartilage health.
- BMP-2 + TGF-β creates a stronger osteogenic signal than either alone.
Potential Clinical Applications
1. Orthopedics & Height Enhancement
- Pediatric short stature: TGF-β agonists + GH/IGF-1 therapy.
- Late-stage growth plate stimulation: Before epiphyseal fusion.
2. Orthognathic & Aesthetic Bone Remodeling
- Maxillary hypoplasia: TGF-β + palatal expanders.
- Mandibular retrognathia: TGF-β + functional appliances.
3. Fracture Healing & Bone Grafting
- Accelerates callus formation when combined with BMP-2/HDACi.
Risks & Limitations
1. Overgrowth & Asymmetry
- Uncontrolled TGF-β may cause heterotopic ossification or uneven bone growth.
2. Fibrotic Side Effects
- Excessive TGF-β can lead to tissue fibrosis (e.g., muscle stiffness, joint scarring).
3. Systemic vs. Localized Delivery
- Local injections (e.g., mandibular condyle) may reduce side effects.
Introduction
Bone Morphogenetic Proteins (BMPs) are master regulators of skeletal formation, playing critical roles in embryonic development and postnatal bone remodeling. As members of the TGF-β superfamily, BMPs stimulate osteoblast differentiation, bone mineralization, and fracture repair. This article explores how BMP agonists enhance osteoblast activity, their effects on bone development, and their therapeutic applications in orthopedics, dentistry, and skeletal regeneration.BMP Signaling and Osteoblast Regulation
1. BMP Receptor Activation
BMPs bind to type I and type II serine/threonine kinase receptors, triggering downstream signaling via:- Smad-dependent pathway (Smad1/5/8 phosphorylation → complex with Smad4 → nuclear translocation)
- Non-Smad pathways (MAPK, PI3K/AKT)
2. Osteoblast Differentiation
BMP signaling drives bone formation by:- Inducing Runx2 and Osterix – Master transcription factors for osteoblast lineage commitment.
- Enhancing ALP and Osteocalcin – Key markers of mature osteoblasts.
- Stimulating Collagen I Synthesis – Essential for bone matrix deposition.
3. Cross-Talk with Other Pathways
- Wnt/β-catenin – BMPs synergize with Wnt to amplify osteogenesis.
- Hedgehog (Ihh) – Critical for endochondral ossification during development.
- IGF-1 & FGF – Enhance BMP-mediated bone formation.
BMP Agonists and Their Effects on Bone Development
1. Natural BMP Ligands
- BMP-2 & BMP-7 (OP-1) – Most studied for osteoinduction; used clinically in spinal fusion and fracture repair.
- BMP-4 & BMP-6 – Also potent, but with varying tissue specificity.
- GDF-5 (BMP-14) – Important for joint and cartilage formation.
2. Synthetic & Small-Molecule BMP Agonists
- KUS121 (a VCP modulator) – Enhances BMP-2-induced osteogenesis.
- Thiazovivin (ROCK inhibitor) – Boosts BMP signaling in mesenchymal stem cells (MSCs).
- Strontium ranelate – Mimics BMP effects by activating calcium-sensing receptors.
3. Effects on Different Bone Types
Long Bones (Height Growth): Stimulates growth plate chondrocytes → endochondral ossificationClavicle (Intramembranous Bone): Directly increases osteoblast-mediated bone deposition
Mandible/Maxilla (Craniofacial Bones): Enhances sutural expansion and condylar growth
Trabecular Bone (Spine/Hips): Improves bone density by increasing osteoblast activity
Therapeutic Applications
1. Orthopedics & Fracture Healing
- FDA-approved BMP-2 (Infuse®) – Used in spinal fusion, tibial non-unions.
- BMP-7 (OP-1) – Approved for recalcitrant long bone fractures.
2. Dental & Maxillofacial Reconstruction
- Alveolar ridge augmentation – BMP-2 accelerates jawbone regeneration.
- Sinus lift procedures – BMP-soaked collagen sponges enhance bone graft success.
3. Osteoporosis & Age-Related Bone Loss
- Local BMP delivery may counteract age-related osteoblast decline.
- Combination with PTH (teriparatide) – Potential for stronger anabolic effects.
Challenges & Limitations
1. Overactive Bone Formation
- Ectopic ossification – Uncontrolled BMP signaling can cause abnormal bone growth in soft tissues.
- Dose-dependent side effects – High BMP doses may lead to inflammation or resorption.
2. Delivery Issues
- Short half-life – Requires carrier systems (e.g., collagen scaffolds, hydrogels).
- Cost – Recombinant BMP therapies are expensive.
3. Alternative Strategies
- BMP gene therapy (e.g., viral vectors encoding BMP-2).
- Small-molecule enhancers (e.g., LDN-193189 derivatives that fine-tune BMPR activity).
Conclusion
BMP agonists are powerful stimulators of osteoblast differentiation and bone formation, with wide-ranging applications in orthopedics, dentistry, and skeletal repair. While challenges like ectopic ossification and high costs remain, advances in targeted delivery and combination therapies (e.g., with HDAC inhibitors or IGF-1) could unlock new treatments for bone defects, osteoporosis, and craniofacial reconstruction. Future research should focus on precision modulation of BMP signaling to maximize efficacy while minimizing risks.The Optimal Bone Growth Stack: Maximizing Osteogenesis with HDAC Inhibitors, Steroids, PTH, and More
Bone growth and remodeling are complex processes influenced by hormonal, genetic, and nutritional factors. For individuals looking to maximize bone density—whether for athletic performance, injury recovery, or combating osteoporosis—a carefully designed stack can significantly enhance osteogenesis. This article explores the most effective compounds and nutrients for bone growth, including HDAC inhibitors (e.g., vorinostat), anabolic steroids (e.g., Anavar), PTH analogs, aromatase inhibitors, growth hormone, macronutrient optimization (protein and carbohydrates), and key vitamins/minerals.1. HDAC Inhibitors (Vorinostat) – Epigenetic Bone Enhancement
Histone deacetylase (HDAC) inhibitors, such as vorinostat (SAHA), have shown promise in promoting osteoblast differentiation and bone formation.- Mechanism: HDAC inhibitors modify gene expression, increasing RUNX2 activity (a key transcription factor for osteoblast differentiation).
- Research: Studies indicate that HDAC inhibition reduces bone resorption while stimulating new bone formation, making it useful for osteoporosis and fracture healing.
- Dosage: Vorinostat is typically used at 50–100 mg/day in clinical settings, but lower doses (10–25 mg) may suffice for bone-specific effects.
2. Anabolic Steroids (Oxandrolone/Anavar) – Strong Bone Stimulation
Anavar (oxandrolone) is one of the best steroids for bone mineral density (BMD) due to its low androgenic side effects and strong anabolic activity.- Mechanism:
- Increases IGF-1 (critical for bone growth).
- Stimulates osteoblasts directly via androgen receptor activation.
- Reduces bone resorption by suppressing osteoclast activity.
- Dosage: 10–20 mg/day is sufficient for bone benefits without significant liver strain.
- Synergy: Combines well with PTH analogs and GH for enhanced bone formation.
3. Parathyroid Hormone (PTH) Analogs – The Gold Standard for Bone Growth
Teriparatide (Forteo) is an FDA-approved PTH(1-34) analog that dramatically increases bone density by stimulating osteoblasts.- Mechanism:
- Intermittent PTH (daily injections) boosts osteoblast activity.
- Increases calcium absorption in the gut and kidneys.
- Dosage: 20 mcg/day subcutaneously (standard protocol).
- Cycling: Limited to 18–24 months due to osteosarcoma risk (rare).
4. Aromatase Inhibitors (AIs) – Epiphyseal plate closure
Inhibiting estrogen is important for preventing/delaying epiphyseal plate closure to ensure that the long bones (arms, legs, spine, clavicles, remain in growth phase for longer.5. Growth Hormone (GH) & IGF-1 – Critical for Bone Elongation & Density
GH and IGF-1 are essential for bone elongation (epiphyseal plate stimulation) and collagen synthesis.- Mechanism:
- GH → ↑ IGF-1 → osteoblast proliferation.
- Enhances calcium retention.
- Dosage:
- 2–4 IU/day (for bone-specific benefits).
- IGF-1 LR3 (20–50 mcg/day) can be used alternatively.
6. Nutrition – The Foundation of Bone Growth
A. High Protein (MTOR Stimulation)
- Mechanism: Leucine activates mTOR, increasing osteoblast activity.
- Dosage: 1.6–2.2 g/kg bodyweight (prioritize whey, collagen, and bone broth).
B. Optimized Carbohydrate Intake (Insulin-Mediated Bone Formation)
- Mechanism:
- Insulin is an anabolic hormone that enhances osteoblast activity and collagen synthesis.
- Carbohydrates post-workout spike insulin, improving nutrient delivery to bones.
- Dosage:
- 3–5 g/kg bodyweight (adjust based on activity level).
- Prioritize peri-workout carbs (e.g., dextrose, rice, oats) for maximal insulin sensitivity.
C. Vitamin D3 + K2 (Osteocalcin Activation)
- D3 (5000–10,000 IU/day) → calcium absorption.
- K2 (MK-4/MK-7) → activates osteocalcin, directing calcium into bones.
D. Magnesium, Zinc, Boron
- Magnesium (400–600 mg/day) → cofactor for bone enzymes.
- Zinc (30–50 mg/day) → collagen synthesis.
- Boron (3–10 mg/day) → reduces calcium excretion.
E. Collagen & Hyaluronic Acid
- Type II collagen (10–20 g/day) supports bone matrix formation.
7. Additional Considerations
A. Mechanical Loading (Weight-Bearing Exercise)
- Resistance training and impact exercises (jumping) stimulate bone remodeling.
B. Progesterone (Potential Synergy)
- Low-dose progesterone may enhance osteoblast activity (needs more research).
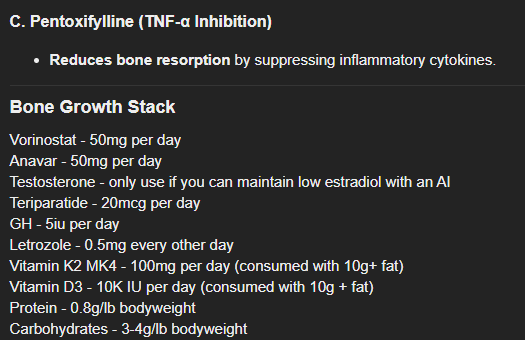
C. Pentoxifylline (TNF-α Inhibition)
- Reduces bone resorption by suppressing inflammatory cytokines.
Bone Growth Stack
Vorinostat - 50mg per dayAnavar - 50mg per day
Testosterone - only use if you can maintain low estradiol with an AI
Teriparatide - 20mcg per day
GH - 5iu per day
Letrozole - 0.5mg every other day
Vitamin K2 MK4 - 100mg per day (consumed with 10g+ fat)
Vitamin D3 - 10K IU per day (consumed with 10g + fat)
Protein - 0.8g/lb bodyweight
Carbohydrates - 3-4g/lb bodyweight
Conclusion
The optimal bone growth stack combines pharmaceutical agents (HDAC inhibitors, PTH, steroids, GH) with targeted nutrition (high protein, strategic carbohydrate intake, D3/K2, collagen). Anavar and teriparatide are particularly potent, while vorinostat offers a novel epigenetic approach. Carbohydrate timing around workouts maximizes insulin’s anabolic effects on bone, while protein and micronutrients provide the building blocks for osteogenesis. Aromatase inhibitors can delay ephiphyseal plate closure which means a longer time for these compounds to exert their effects.For best results, pair this stack with progressive resistance training, adequate recovery, and periodic blood work to monitor biomarkers like IGF-1, estrogen, and calcium levels.
Introduction
Bone is a dynamic tissue that constantly undergoes remodeling—a balance between bone resorption by osteoclasts and bone formation by osteoblasts. While major fractures are easily detectable, micro traumas and micro fractures are small-scale injuries that accumulate over time due to repetitive stress, mechanical loading, or minor impacts. These microscopic damages play a crucial role in bone adaptation and repair, influencing osteoblast activity and overall bone remodeling.What Are Micro Traumas and Micro Fractures?
Micro traumas refer to tiny, often undetectable injuries in bone tissue caused by repetitive stress, such as in athletes or individuals with physically demanding jobs. Micro fractures are slightly more defined, representing small cracks in the bone matrix that do not disrupt overall bone integrity but can weaken the structure if left unrepaired.These micro-damages are common in weight-bearing bones (e.g., tibia, femur) and trabecular bone (spongy bone), where cyclic loading creates stress concentrations. Unlike major fractures, micro fractures do not always cause immediate pain but can lead to chronic conditions like stress fractures or osteoporosis if repair mechanisms fail.
Bone Remodelling and the Role of Osteoblasts
Bone remodelling is a tightly regulated process involving:- Osteoclasts – Break down damaged bone.
- Osteoblasts – Synthesize new bone matrix (osteoid) and promote mineralization.
- Microdamage Detection: Osteocytes (bone’s mechanosensors) detect strain and release signalling molecules (e.g., RANKL, sclerostin).
- Osteoclast Activation: Osteoclasts resorb damaged bone, creating resorption pits.
- Osteoblast Recruitment: Mesenchymal stem cells differentiate into osteoblasts, which deposit new bone.
How Micro Fractures Affect Osteoblasts
- Increased Osteoblast Activity – Small, controlled microdamage stimulates osteoblast proliferation, enhancing bone formation as an adaptive response (Wolff’s Law).
- Chronic Overload and Suppressed Repair – Excessive microdamage without adequate recovery can overwhelm osteoblasts, leading to:
- Accelerated bone loss if resorption outpaces formation.
- Fatigue-induced apoptosis (cell death) of osteoblasts, impairing repair.
- Altered Signalling Pathways – Prolonged stress may dysregulate Wnt/β-catenin (critical for osteoblast differentiation) and increase sclerostin (an osteoblast inhibitor), reducing bone formation.
Clinical Implications
- Stress Fractures – Common in athletes and military recruits due to repetitive microdamage.
- Osteoporosis – Aging or hormonal changes can impair microdamage repair, weakening bone.
- Bone Healing Therapies – Understanding osteoblast responses may improve treatments (e.g., anabolic drugs like teriparatide).
Conclusion
Micro traumas and micro fractures are essential for bone adaptation but can become detrimental if repair mechanisms falter. This means it is important to combine bonesmashing with usage of compounds that increase osteoblasts (PTH analogs, androgens, growth factors). Osteoblasts play a pivotal role in maintaining bone integrity, and their response to microdamage determines whether bone strengthens or deteriorates.Intensity and technique:
Use your fist or another hard/heavy object to hit your facial bones. Do at an intensity that basically is the maximum that you can tolerate - your tolerance will increase over-time due to increased bone density and reduced nerve sensitivity (the same adaptations that happen to muay thai / kickboxing trainers who condition their shins).
Duration and frequency:
Hit a certain area for 1-2 minutes at a high intensity. Start off doing this 1-2 times a week and gauge recovery of your skin and how long the area remains sensitive to touch. Increase the frequency towards every other day as you see fit.
Bracing:
It is extremely important to brace in order to minimize brain movement during bonesmashing. The only reason fighters end up with CTE (chronic traumatic encephalopathy) is because of the movement of their head when punched which causes their brain to rattle around in their skull.
When you are going to begin a bonesmashing session, brace at the very least against your other arm/hand. Optimal bracing is against a seat that supports your head, or bracing by lying down in bed. Bracing against your hand and a hard wall is also effective.
Use your fist or another hard/heavy object to hit your facial bones. Do at an intensity that basically is the maximum that you can tolerate - your tolerance will increase over-time due to increased bone density and reduced nerve sensitivity (the same adaptations that happen to muay thai / kickboxing trainers who condition their shins).
Duration and frequency:
Hit a certain area for 1-2 minutes at a high intensity. Start off doing this 1-2 times a week and gauge recovery of your skin and how long the area remains sensitive to touch. Increase the frequency towards every other day as you see fit.
Bracing:
It is extremely important to brace in order to minimize brain movement during bonesmashing. The only reason fighters end up with CTE (chronic traumatic encephalopathy) is because of the movement of their head when punched which causes their brain to rattle around in their skull.
When you are going to begin a bonesmashing session, brace at the very least against your other arm/hand. Optimal bracing is against a seat that supports your head, or bracing by lying down in bed. Bracing against your hand and a hard wall is also effective.



 what’s the point though? most of the stuff in these guides is water anyway besides maybe androgenic’s. still, gotta mirin the dedication lol.
what’s the point though? most of the stuff in these guides is water anyway besides maybe androgenic’s. still, gotta mirin the dedication lol.