Zagro

Roids over Foids
- Joined
- Aug 19, 2024
- Posts
- 3,721
- Reputation
- 16,371
I suggest you read this thread in dark mode
Disclaimer
The following information I'll provide is only meant for educational purposes and i would advise no one to take anything remotely close to this compound or any compound without medical supervision and prescription. I'm not advising you to take anything or recommending it. Please do not even think of taking any of the compounds I've mentioned in the thread without the proper knowledge or supervision.
Introduction
Welcome to another thread, this time i will be explaining every single aspect of PTH analogues possible. Its been a while since my last thread (HGH 101) as i have been busy with my own stack and researching different topics similar to this. I have 2-3 other threads on the way and will put my best effort in all of them to teach what I've learned and partly for personal gain. I'm always open to questions and advice so feel free to ask whatever, also i recently began doing coaching so if you're intested send me a dm on discord my user is zagronoidv2. This thread t ook a lot of time as i had to begin learning about a whole new topic from scratch but i figured it out in the end.
Related Threads
Here are some other threads with relevance to what i will be discussing today, i would recommend you to also check these out to fully understand the compound before you do anything irreversible.
Threads:
post puberty bone growth guide (teriparatide)
Teriparatide vs Abaloparatide : Which PTH Analog is Better?
Videos:
Teriparatide (Forteo) - Pharmacist Review - Uses, Dosing, Side Effects
Abaloparatide Uses, Dosages, Side Effects & Mechanism | Tymlos
PTH Analogues
Parathyroid Hormone (PTH) analogues are a type of medication that mimic the action of the body's natural parathyroid hormone synthetically. They work by binding to the PTH1 receptor which is the same receptor that your body's natural PTH uses in bone and also kidney. PTH exposure maintains calcium and phosphate balance by increasing calcium reabsorption in the kidney which reduces phosphate reabsorption and stimulates vitamin D activation and also increases bone resorption to release minerals into the blood. On the contrast if PTH stays elevated all the time the bone resorption will overpower and bone will be gradually lost, like hyperparathyroidism which is why ensuring intermittent signaling of PTH to be in a positive remodeling balance is crucial.
The main PTH analogues in clinical use are:
Teriparatide (1-34)
Abaloparatide (1-34)
Recombinant Full-length PTH (1–84)

Teriparatide
Teriparatide is the recombinant form of the first 34 amino acids of human parathyroid hormone which represents the full N-terminal fragment of the hormone. This part is biologically active because it contains the domains that bind and activate the PTH1 receptor (PTH1R). The natural hormone is 84 amino acids long but the C-terminal portion isn't needed for any bone building or calcium regulating actions. The C-terminal interacts with other receptors like C-PTH receptors and their downstream signals are more modest and inhibit osteoclast activity rather than stimulate bone resorption.
In clinics teriparatide is normally used for patients with a high risk of fracture, postmenopausal women and men with severe osteoporosis and also those with glucocorticoid-induced bone loss. It is usually prescribed and advised to use for up to 24 months/2 years your whole life and followed by an antiresorptive drug (like a bisphosphonate or denosumab) to maintain the gains.
Pros & Cons
Like almost every other compound, teriparatide also has its own upsides and downsides which you have to either accept as a trade-off and take the full risk or try to minimise the chance of any adverse effects as much as possible. It’s up to you if you wanna take any risks for your goals as I'm only here to educate you on every possible pro and con you could expect.

Abaloparatide
Abaloparatide is also another recombinant form of the first 34 amino acids of human parathyroid hormone which respresent the full N-terminal fragment of the hormone. Its made to act on the same PTH1 receptor (PTH1R) that both natural PTH and teriparatide act on. Its pretty similar to teriparatide but it has some different mechanisms. The thing that makes abaloparatide special is that it binds to PTH1R in a slightly different conformation preference when compared to teriparatide, it favors the RG conformation (shorter-lived signaling) instead of the R0 conformation (longer-lived). This results in stronger anabolic (bone-building) effects while limiting bone resorption and hypercalcemia.
In clinics abaloparatide is mainly used for postmenopausal women at very high fracture risk, but it's also studied in men and glucocorticoid-induced osteoporosis. The treatment is limited to 24 months maximum in a lifetime (just like teriparatide), after therapy an antiresorptive drug (bisphosphonate or denosumab) to maintain the gains just like teriparatide.
Pros & Cons
Abaloparatide is pretty similar to teriparatide but abaloparatide is the newer and "better" option as it has a few advantages and it is considered safer and has a better side-effect profile compared to teriparatide, although teriparatide is more potent in some aspects and abaloparatide is better in other aspects so like its up to your goals to choose which one you want to use.

Recombinant Full-Length PTH
I will not be explaining this one in-depth as teriparatide and abaloparatide are superior for bone building. The reason for the 1-34 PTH analogues being superior is because they are far more studied with more data, the actual "anabolic" part is the N-terminal so adding the C-terminal hasn't shown a clinical anabolic advantage over the N-terminal alone. To add on, recombinant full-length PTH analogue 1-84 is only approved for hypoparathyroidism by FDA and not something like osteoporosis. Getting the PTH analogue itself is a pain in the ass too as the producers of Natpara (Recombinant Full-Length PTH Analogue) have announced that they globally discontinued its manufacturing. There is also no evidence for it being safer or "better" in any way.
Usages
As I've said PTH analogue's main clinical use is on women with high fracture risk, postmenopausal women and women/men with osteoporosis, its uses for anything else isn't heavily studied so its mostly theoretical and the risks are up to you although i wouldn't advise its usage and surely don't ever touch it if you aren't familiar with the compound or any compound at all. My own use for teriparatide is its particular effects on bone tissue and bone-building cells which is perfectly what I'm looking for. In theory this compound will help bone remodeling and any healing process that's for sure but it's effects on bone growth by itself should moderate or at the least minimal but trying doesn't hurt, also my reasoning is because of teriparatide's cellular/molecular pros. It should also potentially synergise well with other peptides and steroids used in a usual "heightmaxxing" stack, so i see potential in PTH analogues and will use them myself.

Dosages
The dosages vary for the main PTH analogues but the clinical approved ones and the doses used on most patients are; 20µg for teriparatide, 80µg for abaloparatide and 100µg for recombinant full-length PTH. This doesn't mean that going above any of these doses is lethal or that their effects become diminishing it actually becomes even more potent most of the time and you can still keep a positive remodeling balance without it tipping into bone loss, although it isn't recommended as it carries even more risks and the rare side effects become much more realistic and probable.
For teriparatide for example , this means that as the doses increase it becomes even more potent but after a certain point which is the "anabolic window" if the exposure is too high or too continous (not intermittently dosed) bone resorption overweights bone formation and it results in net bone loss, so its either "anabolic" or "catabolic". While the usual 20µg dose is very potent itself you can always increase the dose to an amount like 40µg which makes the pros even more significant but it comes with more of the common adverse effects that I've explained in the thread, but it still keeps you in that "anabolic" state. Some countries like Japan use once-weekly injections of 56.5µg teriparatide instead of the daily injections. At last i would suggest you use 20µg instead of the higher doses at the beginning and if you know what you're doing and respond well then you can think about upping the dose up to 40µg.
For abaloparatide it has also been shown that it exhibits dose-dependent anabolic effects on bone, that means as the dose increases it becomes even more potent just like teriparatide. The way abaloparatide binds to the PTH1 receptors favoring the RG conformation means it produces shorter and more temporary bursts of signaling. It's bias allows it to become even more potent than teriparatide but still have less adverse effects and less drive towards bone resorption. The usual and approved dose is 80µg daily which led to very rapid and significant gains in clinical trials, although lower doses like 40µg were also studied it did give improvements on bone but of course the 80µg dose was far superior without many sides added. Doses above 80µg haven't been studied yet as abaloparatide already exhibits a strong anabolic response with minimal side effect profile but in theory it should be safer to dose abaloparatide higher cause of it's conformation bias.

Costs & Sourcing
The costs largely depend on where you're getting it from but aren't unrealistic if we choose a Chinese manufacturer which provides the raw powder of the compound which you then have to put in vials yourself, another choice you have is getting it in vials but the costs do rise in that case. The best choice is getting it from a research institution as that will almost fully guarantee sterility and purity but they require proof of you being an actual researcher or that you own a research institution yourself. One source that is quite publicly known around the forum is Indiamart, you can also find some of the PTH analogues there like teriparatide although the prices are moderate the safety isn't guaranteed as you're buying it from an almost random vendor but it is pharmaceutical grade (Teriparatide Link). As you can see 600 mcg of teriparatide costs 25,000 Rupees which converts to around €250/$290/£210 for a 30 day supply of teriparatide.
Look around for other vendors and find the best one that suits your budget but be sure to check the seller's reviews and "rank" on the site itself. Another thing you should look out for is if the compound will actually get delivered and not seized as some countries are strict with customs, check your country's law and ask the seller himself. For me any shipment directly from India to the Netherlands gets seized instantly, what you can do is ask the seller for any other shipping method and one that ships to another EU country first to ensure the shipping is from another EU country to your own homeland that way the shipping is almost guaranteed to be received by you. You can also do your own research and find a seller yourself but be mindful and don't get yourself scammed in the end and watch out for some of the dropshippers.
Thank you for reading (if you even have read this monstrosity) this took me a long amount of time as i had to learn all this myself and as i learnt more i had to update the thread, but now i will be working on my next thread which will be on HDACi and i hope this thread has helped you in any way.
Tags: @menas @Sadist @chadisbeingmade @SlayerJonas @Bitchwhipper2
Disclaimer
The following information I'll provide is only meant for educational purposes and i would advise no one to take anything remotely close to this compound or any compound without medical supervision and prescription. I'm not advising you to take anything or recommending it. Please do not even think of taking any of the compounds I've mentioned in the thread without the proper knowledge or supervision.
Introduction
Welcome to another thread, this time i will be explaining every single aspect of PTH analogues possible. Its been a while since my last thread (HGH 101) as i have been busy with my own stack and researching different topics similar to this. I have 2-3 other threads on the way and will put my best effort in all of them to teach what I've learned and partly for personal gain. I'm always open to questions and advice so feel free to ask whatever, also i recently began doing coaching so if you're intested send me a dm on discord my user is zagronoidv2. This thread t ook a lot of time as i had to begin learning about a whole new topic from scratch but i figured it out in the end.
Related Threads
Here are some other threads with relevance to what i will be discussing today, i would recommend you to also check these out to fully understand the compound before you do anything irreversible.
Threads:
post puberty bone growth guide (teriparatide)
Teriparatide vs Abaloparatide : Which PTH Analog is Better?
Videos:
Teriparatide (Forteo) - Pharmacist Review - Uses, Dosing, Side Effects
Abaloparatide Uses, Dosages, Side Effects & Mechanism | Tymlos
PTH Analogues
Parathyroid Hormone (PTH) analogues are a type of medication that mimic the action of the body's natural parathyroid hormone synthetically. They work by binding to the PTH1 receptor which is the same receptor that your body's natural PTH uses in bone and also kidney. PTH exposure maintains calcium and phosphate balance by increasing calcium reabsorption in the kidney which reduces phosphate reabsorption and stimulates vitamin D activation and also increases bone resorption to release minerals into the blood. On the contrast if PTH stays elevated all the time the bone resorption will overpower and bone will be gradually lost, like hyperparathyroidism which is why ensuring intermittent signaling of PTH to be in a positive remodeling balance is crucial.
The main PTH analogues in clinical use are:
Teriparatide (1-34)
Abaloparatide (1-34)
Recombinant Full-length PTH (1–84)

Teriparatide
Teriparatide is the recombinant form of the first 34 amino acids of human parathyroid hormone which represents the full N-terminal fragment of the hormone. This part is biologically active because it contains the domains that bind and activate the PTH1 receptor (PTH1R). The natural hormone is 84 amino acids long but the C-terminal portion isn't needed for any bone building or calcium regulating actions. The C-terminal interacts with other receptors like C-PTH receptors and their downstream signals are more modest and inhibit osteoclast activity rather than stimulate bone resorption.
In clinics teriparatide is normally used for patients with a high risk of fracture, postmenopausal women and men with severe osteoporosis and also those with glucocorticoid-induced bone loss. It is usually prescribed and advised to use for up to 24 months/2 years your whole life and followed by an antiresorptive drug (like a bisphosphonate or denosumab) to maintain the gains.
Pros & Cons
Like almost every other compound, teriparatide also has its own upsides and downsides which you have to either accept as a trade-off and take the full risk or try to minimise the chance of any adverse effects as much as possible. It’s up to you if you wanna take any risks for your goals as I'm only here to educate you on every possible pro and con you could expect.
Pros
Bone Builder: Most of the drugs that are prescribed for osteoporosis like bisphosphonates (alendronate and zoledronic acid for example) and denosumab works mainly by slowing down bone resorption. Their mechanism works by inhibiting the activity of osteoclasts which are the cells that actually break down and recycle bone tissue. On the other hand teriparatide uses a completely different mechanism and instead of just preventing bone loss its actually a bone-building agent and actually builds new bone mainly by stimulating osteoblasts which are the bone forming cells.
Study (1)
Positive Remodeling Balance: This means that during each bone remodeling cycle more bone is formed than resorbed. Intermittent signaled usage of teriparatide drives this by boosting osteoblast activity and survival more than osteoclast resorption, resulting in a net gain of bone mas, stronger microarchitecture and reduced fracture risk.
Study (1)
Fracture Risk Reduction: This refers to teriparatide’s ability to make bones stronger and less likely to break. By stimulating new bone formation, improving trabecular thickness and just enhancing overall bone quality. Teriparatide lowers the chance of fractures as clinical trials have shown about a 65% reduction in vertebral fractures and nearly 50% reduction in non-vertebral fractures. This makes it one of the most effective treatments for preventing fractures in patients with severe osteoporosis.
Study (1)
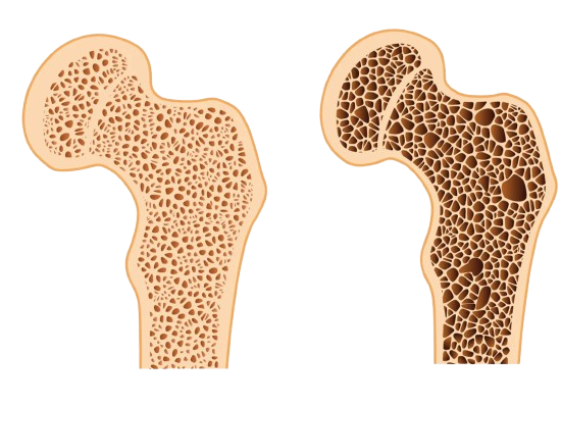
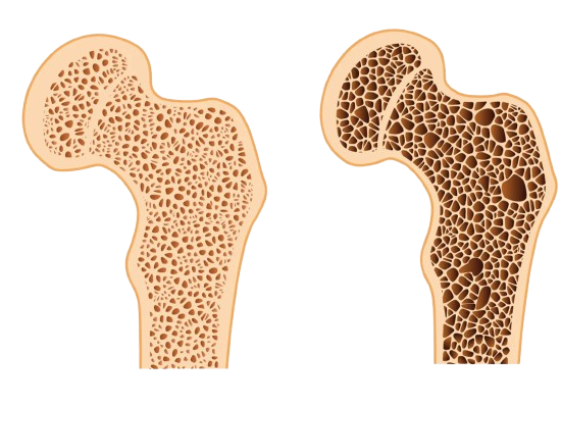
Trabecular Bone Strength: Another upside of teriparatide is its ability to strengthen the trabecular bone, that is the quality and resilience of the inner spongy bone found in the spine, pelvis and ends of long bones like the femur. With osteoporosis trabeculae becomes thin, disconnected and also fragile which just makes it significantly weaker than normal. Teriparatide restores the trabecular structure by thickening existing trabeculae and reconnects the disconnected and broken struts. This restores the bone and imrpoves the bone's ability to absorb mechanical stress making it more resistant to fractures.
Study (1) (Same study as the one for fracture risk reduction)

Fracture Healing: With teriparatide fracture healing is faster and stronger because it stimulates chondrocytes and osteoblasts, increases collagen and growth factor production and enhances blood supply at the fracture site. This leads to quicker callus formation, better mineralization and faster remodeling into strong bone especially in osteoporotic patients.
Study (1)
BMD Gains: with teriparatide BMD Gains are rapid and significant because it directly stimulates new bone formation. Increases in spine bone mineral density can be seen within 3-6 months of proper usage, often faster than with antiresorptive drugs. Its not only gains in mineral but also improvement in bone quality and structure resulting in stronger and more fracture-resistant bone tissue.
Study (1)
Cellular/Molecular Benefits
PTH1R Activation (N-terminal binding): Teriparatide is the active N-terminal 1-34 fragment of PTH which binds to the PTH1 receptor (PTH1R) on osteoblasts, osteocytes and kidney cells. PTH1R is a G-protein coupled receptor that activates cAMP/PKA and PLC/PKC pathways. In bone tissue this stimulates osteoblast survival and activity and in the kidney it regulates calcium and phosphate balance.
Suppression of Sclerostin: Osteocytes normally secrete sclerostin which is a protein that inhibits the Wnt/β-catenin pathway, which is very critical for bone formation. Teriparatide decreases sclerostin expression and that means it makes Wnt signaling extra potent. This all results in more osteoblast proliferation, survival and bone matrix production.
Higher IGF-1 and VEGF Production: IGF-1 (Insulin-Like Growth Factor 1) gets stimulated by teriparatide in osteoblasts and that promotes proliferation, differentiation and survival of bone-forming cells. On the other hand VEGF (Vascular Endothelial Growth Factor) increases under teriparatide and it enhances angiogenesis at remodeling sites which improves nutrient and oxygen delivery to bone tissue. Both of these help moderate to significantly with fracture healing and anabolic remodeling.
RANKL/OPG Modulation: Osteoblasts produce RANKL which activates osteoclasts and osteoprotegerin (OPG), and that blocks RANKL. Teriparatide increases RANKL expression but under intermittent dosing the osteoblast activity outweighs osteclast resorption. This creates a positive remodeling balance which I've talked about a lot in this thread.
Collagen Synthesis Prevents Osteoblast Apoptosis: Osteoblasts that are under PTH signaling ramp up the production of type I collagen which is the main structural protein of bone. Collagen fibers are the ones forming the organic scaffold into which minerals like calcium hydroxyapatite are deposited, resulting in both tensile strenght and rigidity in bone. To add on osteoblasts normally have a limited lifespan and undergo apoptosis (programmed cell death almost like suicide). Teriparatide signaling through cAMP/PKA pathways prolongs osteoblast survival. This means the existing osteoblast just keep producing bone for a longer amount of time and are more balanced towards net formation.
Reactivates Quiescent Bone-Lining Cells: Bone surfaces are mostly covered by flattened and inactive lining cells (osteoblasts). Teriparatide can reactivate these cells and turn them back into working and active osteoblasts that are again able to produce matrix. This results in more bone-building cells and makes bone surfaces more "active".
Stimulates MSC Differentiation: Mesenchymal stem cells (MSCs) in bone marrow can differentiate into osteoblasts, chondrocytes or adipocytes. Teriparatide focuses MSC differentiation toward the osteoblast lineage instead of fat cells. This refreshes the osteoblast population and boosts bone regeneration capacity.
Enhances Osteoblast Activity: Teriparatide directly increases osteoblast matrix production rate (collagen, osteocalcin and alkaline phosphatase activity). This helps with mineralizzation and deposition of new bone tissue.
Improves Osteocyte Function: PTH signaling enhances osteocyte's ability to detect strain and coordinate remodeling. It reduces osteocyte apoptosis and suppresses screlostin and help sustain healthy bone architecture and mechanical responsiveness.
Promotes Chondrocyte Recruitment: During fracture repairment and bone growht processes, cartilage-forming cells (chondrocytes) create a scaffold (soft callus) before mineralization. Teriparatide stimulates chondrocyte recruitment and differentiation that enhances endochondral ossification and speeds up fracture healing.
Bone Builder: Most of the drugs that are prescribed for osteoporosis like bisphosphonates (alendronate and zoledronic acid for example) and denosumab works mainly by slowing down bone resorption. Their mechanism works by inhibiting the activity of osteoclasts which are the cells that actually break down and recycle bone tissue. On the other hand teriparatide uses a completely different mechanism and instead of just preventing bone loss its actually a bone-building agent and actually builds new bone mainly by stimulating osteoblasts which are the bone forming cells.
Study (1)
Positive Remodeling Balance: This means that during each bone remodeling cycle more bone is formed than resorbed. Intermittent signaled usage of teriparatide drives this by boosting osteoblast activity and survival more than osteoclast resorption, resulting in a net gain of bone mas, stronger microarchitecture and reduced fracture risk.
Study (1)
Fracture Risk Reduction: This refers to teriparatide’s ability to make bones stronger and less likely to break. By stimulating new bone formation, improving trabecular thickness and just enhancing overall bone quality. Teriparatide lowers the chance of fractures as clinical trials have shown about a 65% reduction in vertebral fractures and nearly 50% reduction in non-vertebral fractures. This makes it one of the most effective treatments for preventing fractures in patients with severe osteoporosis.
Study (1)
Trabecular Bone Strength: Another upside of teriparatide is its ability to strengthen the trabecular bone, that is the quality and resilience of the inner spongy bone found in the spine, pelvis and ends of long bones like the femur. With osteoporosis trabeculae becomes thin, disconnected and also fragile which just makes it significantly weaker than normal. Teriparatide restores the trabecular structure by thickening existing trabeculae and reconnects the disconnected and broken struts. This restores the bone and imrpoves the bone's ability to absorb mechanical stress making it more resistant to fractures.
Study (1) (Same study as the one for fracture risk reduction)

Fracture Healing: With teriparatide fracture healing is faster and stronger because it stimulates chondrocytes and osteoblasts, increases collagen and growth factor production and enhances blood supply at the fracture site. This leads to quicker callus formation, better mineralization and faster remodeling into strong bone especially in osteoporotic patients.
Study (1)
BMD Gains: with teriparatide BMD Gains are rapid and significant because it directly stimulates new bone formation. Increases in spine bone mineral density can be seen within 3-6 months of proper usage, often faster than with antiresorptive drugs. Its not only gains in mineral but also improvement in bone quality and structure resulting in stronger and more fracture-resistant bone tissue.
Study (1)
Cellular/Molecular Benefits
PTH1R Activation (N-terminal binding): Teriparatide is the active N-terminal 1-34 fragment of PTH which binds to the PTH1 receptor (PTH1R) on osteoblasts, osteocytes and kidney cells. PTH1R is a G-protein coupled receptor that activates cAMP/PKA and PLC/PKC pathways. In bone tissue this stimulates osteoblast survival and activity and in the kidney it regulates calcium and phosphate balance.
Suppression of Sclerostin: Osteocytes normally secrete sclerostin which is a protein that inhibits the Wnt/β-catenin pathway, which is very critical for bone formation. Teriparatide decreases sclerostin expression and that means it makes Wnt signaling extra potent. This all results in more osteoblast proliferation, survival and bone matrix production.
Higher IGF-1 and VEGF Production: IGF-1 (Insulin-Like Growth Factor 1) gets stimulated by teriparatide in osteoblasts and that promotes proliferation, differentiation and survival of bone-forming cells. On the other hand VEGF (Vascular Endothelial Growth Factor) increases under teriparatide and it enhances angiogenesis at remodeling sites which improves nutrient and oxygen delivery to bone tissue. Both of these help moderate to significantly with fracture healing and anabolic remodeling.
RANKL/OPG Modulation: Osteoblasts produce RANKL which activates osteoclasts and osteoprotegerin (OPG), and that blocks RANKL. Teriparatide increases RANKL expression but under intermittent dosing the osteoblast activity outweighs osteclast resorption. This creates a positive remodeling balance which I've talked about a lot in this thread.
Collagen Synthesis Prevents Osteoblast Apoptosis: Osteoblasts that are under PTH signaling ramp up the production of type I collagen which is the main structural protein of bone. Collagen fibers are the ones forming the organic scaffold into which minerals like calcium hydroxyapatite are deposited, resulting in both tensile strenght and rigidity in bone. To add on osteoblasts normally have a limited lifespan and undergo apoptosis (programmed cell death almost like suicide). Teriparatide signaling through cAMP/PKA pathways prolongs osteoblast survival. This means the existing osteoblast just keep producing bone for a longer amount of time and are more balanced towards net formation.
Reactivates Quiescent Bone-Lining Cells: Bone surfaces are mostly covered by flattened and inactive lining cells (osteoblasts). Teriparatide can reactivate these cells and turn them back into working and active osteoblasts that are again able to produce matrix. This results in more bone-building cells and makes bone surfaces more "active".
Stimulates MSC Differentiation: Mesenchymal stem cells (MSCs) in bone marrow can differentiate into osteoblasts, chondrocytes or adipocytes. Teriparatide focuses MSC differentiation toward the osteoblast lineage instead of fat cells. This refreshes the osteoblast population and boosts bone regeneration capacity.
Enhances Osteoblast Activity: Teriparatide directly increases osteoblast matrix production rate (collagen, osteocalcin and alkaline phosphatase activity). This helps with mineralizzation and deposition of new bone tissue.
Improves Osteocyte Function: PTH signaling enhances osteocyte's ability to detect strain and coordinate remodeling. It reduces osteocyte apoptosis and suppresses screlostin and help sustain healthy bone architecture and mechanical responsiveness.
Promotes Chondrocyte Recruitment: During fracture repairment and bone growht processes, cartilage-forming cells (chondrocytes) create a scaffold (soft callus) before mineralization. Teriparatide stimulates chondrocyte recruitment and differentiation that enhances endochondral ossification and speeds up fracture healing.
Cons
Cortical Bone Caveate: Teriparatide strongly improves trabecular (spongy) bone like in the spine, but in cortical (compact) bone such as the long bone shafts it can initially cause more porosity. This happens because turnover rises on the surface before new bone fully fills in. The effect is usually temporary and is corrected when treatment is followed by an antiresorptive drug.
Study (1)
Losing Bone Gains: The benefits of teriparatide don’t last if therapy stops without a follow up. Bone density and BMD gained during treatment can decline within 1-2 years, and fracture protection weakens. To preserve these gains treatment must be followed by an antiresorptive like a bisphosphonate or denosumab, which “locks in” the new bone.
Study (1)
Common Side Effects

 www.drugs.com
www.drugs.com
Hypercalcemia: Teriparatide injections cause a mild and temporary rise in serum calcium in some patients, they peak 4-6 hours after injection and return to normal levels by 16-24 hours. This happens because teriparatide increases calcium release from bone and enchances intestinal absorption indirectly. The increase is most the time small but in sensitive patients/individuals it causes common symptoms like fatigue, nausea, constipation and muscle weakness. Severe hypercalcemia isn't that common but be sure to monitor calcium levels as you probably don't know if you're at higher risk.
Study (1) Report (1)
Nausea: Its a common reported side effect of teriparatide and its usually pretty mild and short-lived, it occurs within the first few hours after injection. The exact cause isn't really understood but it is possibly linked to temporary shifts in calcium metabolism and possible central nervous system sensivity to these changes.
Report (1) Report (2)
Headache: Some patients also report headaches particularly during the first few weeks of teriparatide usage. The headaches are pretty mild to moderate and tend to stop as the body adapts to daily injections. The cause may be related to changes in vascular tone or fluctuations in calcium and phosphate levels.
Report (1)
Muscle Cramping: This is also another side effects that occasionally gets reported. This is probably linked to altered calcium and electrolyte handling in muscle fibers, since calcium plays a role in muscle contraction and relaxation. They aren't really persistent and can be minimised with hydration.
Report (1)
Joint Pain: Increased bone turnover can cause temporary stress in joints leading to mild joint pain in some patients. This reflects the body's adjustment to active bone remodeling rather than joint damage, its pretty manageable and it stops with time.
Report (1)
Fatigue: Some patients also experience tiredness or a feeling of low energy, it usually occurs early in therapy. It is temporary and stops as the body adapts to new metabolic activity. A good amount of calcium and vitamind D intake may help minimise this side.
Report (1)
Rare Side Effects
Hyperuricemia: Teriparatide can increase uric acid levels in the blood likely through changes in mineral metabolism and kidney handling. In most patients this rise is mild but in those with a history of gout or kidney stones it may trigger gout flares. Clinically significant cases are uncommon and monitoring may be considered in higher-risk individuals.
Calciphylaxis: This is a pretty rare but serious side reported in some patients on teriparatide and it mostly occurs in those with severe kidney disease or advanced vascular pathology. It happens when calcium deposits abnormally in small blood vessels of the skin and fat resulting in painful skin ulcers, necrosis and risk of infection. The condition is also life threatening if untreated so you need to take this serious.
Hypercalciuria: Something that happens with elevated blood calcium is that, its called hypercalciuria and occurs because the kidneys filter out the extra calcium mobilized from bone. If it stays elevated this can predispose to nephrolithiasis (kidney stones), the risk is higher in patients with a history of stones or renal impairments. Although it isn't that extreme and most cases are mild sometimes clinicians do choose to monitor urine calcium and advise enough hydration to reduce the risk.
Orthostatic Hypotension: Whilst the first few injections some patients do notice lightheadedness or dizziness when standing up. This happens cause of the orthostatic hypotension which is basically a temporary drop in blood pressure that likely results from vasodilatory effects of teriparatide's signaling. It lasts a few minutes and doesn't occur with continued use but it’s advised to do the first few injections while seated.
Cortical Bone Caveate: Teriparatide strongly improves trabecular (spongy) bone like in the spine, but in cortical (compact) bone such as the long bone shafts it can initially cause more porosity. This happens because turnover rises on the surface before new bone fully fills in. The effect is usually temporary and is corrected when treatment is followed by an antiresorptive drug.
Study (1)
Losing Bone Gains: The benefits of teriparatide don’t last if therapy stops without a follow up. Bone density and BMD gained during treatment can decline within 1-2 years, and fracture protection weakens. To preserve these gains treatment must be followed by an antiresorptive like a bisphosphonate or denosumab, which “locks in” the new bone.
Study (1)
Common Side Effects

Teriparatide: Uses, Dosage, Side Effects, Warnings - Drugs.com
Teriparatide injection is used to treat osteoporosis in specific men and postmenopausal women who are at high risk for bone fractures. Includes tirparatide side effects, interactions, and indications.
Hypercalcemia: Teriparatide injections cause a mild and temporary rise in serum calcium in some patients, they peak 4-6 hours after injection and return to normal levels by 16-24 hours. This happens because teriparatide increases calcium release from bone and enchances intestinal absorption indirectly. The increase is most the time small but in sensitive patients/individuals it causes common symptoms like fatigue, nausea, constipation and muscle weakness. Severe hypercalcemia isn't that common but be sure to monitor calcium levels as you probably don't know if you're at higher risk.
Study (1) Report (1)
Nausea: Its a common reported side effect of teriparatide and its usually pretty mild and short-lived, it occurs within the first few hours after injection. The exact cause isn't really understood but it is possibly linked to temporary shifts in calcium metabolism and possible central nervous system sensivity to these changes.
Report (1) Report (2)
Headache: Some patients also report headaches particularly during the first few weeks of teriparatide usage. The headaches are pretty mild to moderate and tend to stop as the body adapts to daily injections. The cause may be related to changes in vascular tone or fluctuations in calcium and phosphate levels.
Report (1)
Muscle Cramping: This is also another side effects that occasionally gets reported. This is probably linked to altered calcium and electrolyte handling in muscle fibers, since calcium plays a role in muscle contraction and relaxation. They aren't really persistent and can be minimised with hydration.
Report (1)
Joint Pain: Increased bone turnover can cause temporary stress in joints leading to mild joint pain in some patients. This reflects the body's adjustment to active bone remodeling rather than joint damage, its pretty manageable and it stops with time.
Report (1)
Fatigue: Some patients also experience tiredness or a feeling of low energy, it usually occurs early in therapy. It is temporary and stops as the body adapts to new metabolic activity. A good amount of calcium and vitamind D intake may help minimise this side.
Report (1)
Rare Side Effects
Hyperuricemia: Teriparatide can increase uric acid levels in the blood likely through changes in mineral metabolism and kidney handling. In most patients this rise is mild but in those with a history of gout or kidney stones it may trigger gout flares. Clinically significant cases are uncommon and monitoring may be considered in higher-risk individuals.
Calciphylaxis: This is a pretty rare but serious side reported in some patients on teriparatide and it mostly occurs in those with severe kidney disease or advanced vascular pathology. It happens when calcium deposits abnormally in small blood vessels of the skin and fat resulting in painful skin ulcers, necrosis and risk of infection. The condition is also life threatening if untreated so you need to take this serious.
Hypercalciuria: Something that happens with elevated blood calcium is that, its called hypercalciuria and occurs because the kidneys filter out the extra calcium mobilized from bone. If it stays elevated this can predispose to nephrolithiasis (kidney stones), the risk is higher in patients with a history of stones or renal impairments. Although it isn't that extreme and most cases are mild sometimes clinicians do choose to monitor urine calcium and advise enough hydration to reduce the risk.
Orthostatic Hypotension: Whilst the first few injections some patients do notice lightheadedness or dizziness when standing up. This happens cause of the orthostatic hypotension which is basically a temporary drop in blood pressure that likely results from vasodilatory effects of teriparatide's signaling. It lasts a few minutes and doesn't occur with continued use but it’s advised to do the first few injections while seated.

Abaloparatide
Abaloparatide is also another recombinant form of the first 34 amino acids of human parathyroid hormone which respresent the full N-terminal fragment of the hormone. Its made to act on the same PTH1 receptor (PTH1R) that both natural PTH and teriparatide act on. Its pretty similar to teriparatide but it has some different mechanisms. The thing that makes abaloparatide special is that it binds to PTH1R in a slightly different conformation preference when compared to teriparatide, it favors the RG conformation (shorter-lived signaling) instead of the R0 conformation (longer-lived). This results in stronger anabolic (bone-building) effects while limiting bone resorption and hypercalcemia.
In clinics abaloparatide is mainly used for postmenopausal women at very high fracture risk, but it's also studied in men and glucocorticoid-induced osteoporosis. The treatment is limited to 24 months maximum in a lifetime (just like teriparatide), after therapy an antiresorptive drug (bisphosphonate or denosumab) to maintain the gains just like teriparatide.
Pros & Cons
Abaloparatide is pretty similar to teriparatide but abaloparatide is the newer and "better" option as it has a few advantages and it is considered safer and has a better side-effect profile compared to teriparatide, although teriparatide is more potent in some aspects and abaloparatide is better in other aspects so like its up to your goals to choose which one you want to use.
Pros
Bone Builder: comparable to teriparatide, abaloparatide also is another anabolic osteoporosis treatment meaning it stimulates osteoblast activity which builds new bone instead of just preventing resorption. Its mechanism centers on selective activation of PTH1 receptors (PTH1R) in a way that favors bone formation over resorption so just like positive remodeling balance.
Study (1)
Positive Remodeling Balance: Abaloparatide increases osteoblast number and activity more than osteoclast activity which results in a net gain in bone mass and improved microarchitecture. Intermittent dosing preserves this anabolic state.
Fracture Risk Reduction: Clinical trials have shown that abaloparatide significantly reduced vertebral fractures, non-vertebral fractures and major fractures. These reductions are comparable and somtimes slightly greater than teriparatide.
Study (1)
Trabecular and Cortical Bone Strength: Abaloparatide improves both trabecular spongy bone and cortical compact bone. It works differently compared to teriparatide though cause sometimes teriparatide increases cortical porosity early in therapy and abaloparatide appears to preserve or even enhance cortical bone density and structure.
Study (1)
BMD Gains: Based on clinical trial results abaloparatide produces rapid and large increases in BMD and particularly in the spine and hip, and in the ACTIVE trial at 18 months lumbar spine BMD increased by 9.2% with abaloparatide and 7.4% with teriparatide and the hip BMD gains were also slightly higher than of teriparatide.
Study (1)
Reduced Hypercalcemia Risk: Abaloparatide also has lower rates of hypercalcemia compared to teriparatide and this is due to the differences in mechanisms and how it interacts with PTH1R (it prefarably binds to the receptors's RG conformation which leads to less sustained calcium release).
Study (1)
RG and R0 Conformation: One key difference is that teriparatide binds to PTH1R and stabilizes the R0 conformation which produces longer-lasting cAMP signaling. This results in a strong anabolic response but also increases osteoclast activation and calcium mobilization, which is why more hypercalcemia and cortical porosity is occures early in therapy. On the other hand abaloparatide binds preferably to the RQ conformation which produces shorter and transient signaling, this means it more biased towards osteoblast activation with less osteoclast stimulation and lower calcium release.
Study (1)
Cellular/Molecular Benefits
PTH1R Activation (N-terminal binding): Abaloparatide is a synthetic analogue of the N-terminal PTHrP fragment 1-34 that binds to the PTH1 receptor on osteoblasts, osteocytes and kidney cells. It also activates cAMP/PKA and PLC/PKC pathways but with a bias on temporary binding to the RG conformation of PTH1R, this produces stronger "anabolic" signaling with less resorption compared to teriparatide.
Supression of Sclerostin: Abaloparatide reduces screlostin expression in osteocytes which boosts Wnt/β-catenin signaling. This improves osteoblast proliferation, matrix synthesis and also bone formation itself while reducing inhibition of anabolic pathways.
Higher IGF-1 and VEGF Production: Abaloparatide increases the production of important pathways like IGF-1 and VEGF which are both crucial for bone growth purposes.
RANKL/OPG Modulation: Abaloparatide increases RANKL expression in osteoblasts which stimulates osteoclastogenesis, but because of its transient/temporary receptor binding and intermittent dosing the osteoblast driven bone formation overweights bone resorption. This shifts remodeling towards net anabolic gain with a lower risk profile compared to teriparatide.
Collagen Synthesis and Osteoblast Survival: Abaloparatide stimulates type I collagen synthesis in osteoblasts which provides the structural framework for mineral deposition which is important for bones. To add on cAMP/PKA signaling prolongs osteoblast lifespan by inhibiting apoptosis (programmed cell death) which also results in more sustained bone matrix production.
Reactivation of Quiescent Bone Lining Cells: Bone lining cells on quiescent surfaces can be reactivated or literally "woken up" by abaloparatide to resume matrix secretion and contribute to surface based bone formation. This increases the amount of active bone-forming cells and helps to reactivate them on previously inactive bone surfaces
Stimulation of MSC Differentiation: Abaloparatide promotes mesenchymal stem cell (MSC) differentiation toward the osteoblast lineage also
reduces adipogenesis in bone marrow and refreshing the osteoblast pool for long term bone formation capacity.
Enhanced Osteoblast Activity: Osteoblasts which are exposed to abaloparatide show increased synthesis of collagen, osteocalcin and alkaline phosphatase activity. All of which are very important for mineralization and robust bone matrix deposition.
Improved Osteocyte Function: Abaloparatide signaling reduces osteocyte apoptosis and suppresses sclerostin further which strenghtens the ability of osteocytes to sense strain and regulate remodeling.
Promotion of Chondrocyte Recruitment: Abaloparatide supports chondrocyte recruitment and differentiation during fracture and growth which enhances endochondral ossification. This accelerates callus formation, mineralization and fracture repair.
Bone Builder: comparable to teriparatide, abaloparatide also is another anabolic osteoporosis treatment meaning it stimulates osteoblast activity which builds new bone instead of just preventing resorption. Its mechanism centers on selective activation of PTH1 receptors (PTH1R) in a way that favors bone formation over resorption so just like positive remodeling balance.
Study (1)
Positive Remodeling Balance: Abaloparatide increases osteoblast number and activity more than osteoclast activity which results in a net gain in bone mass and improved microarchitecture. Intermittent dosing preserves this anabolic state.
Fracture Risk Reduction: Clinical trials have shown that abaloparatide significantly reduced vertebral fractures, non-vertebral fractures and major fractures. These reductions are comparable and somtimes slightly greater than teriparatide.
Study (1)
Trabecular and Cortical Bone Strength: Abaloparatide improves both trabecular spongy bone and cortical compact bone. It works differently compared to teriparatide though cause sometimes teriparatide increases cortical porosity early in therapy and abaloparatide appears to preserve or even enhance cortical bone density and structure.
Study (1)
BMD Gains: Based on clinical trial results abaloparatide produces rapid and large increases in BMD and particularly in the spine and hip, and in the ACTIVE trial at 18 months lumbar spine BMD increased by 9.2% with abaloparatide and 7.4% with teriparatide and the hip BMD gains were also slightly higher than of teriparatide.
Study (1)
Reduced Hypercalcemia Risk: Abaloparatide also has lower rates of hypercalcemia compared to teriparatide and this is due to the differences in mechanisms and how it interacts with PTH1R (it prefarably binds to the receptors's RG conformation which leads to less sustained calcium release).
Study (1)
RG and R0 Conformation: One key difference is that teriparatide binds to PTH1R and stabilizes the R0 conformation which produces longer-lasting cAMP signaling. This results in a strong anabolic response but also increases osteoclast activation and calcium mobilization, which is why more hypercalcemia and cortical porosity is occures early in therapy. On the other hand abaloparatide binds preferably to the RQ conformation which produces shorter and transient signaling, this means it more biased towards osteoblast activation with less osteoclast stimulation and lower calcium release.
Study (1)
Cellular/Molecular Benefits
PTH1R Activation (N-terminal binding): Abaloparatide is a synthetic analogue of the N-terminal PTHrP fragment 1-34 that binds to the PTH1 receptor on osteoblasts, osteocytes and kidney cells. It also activates cAMP/PKA and PLC/PKC pathways but with a bias on temporary binding to the RG conformation of PTH1R, this produces stronger "anabolic" signaling with less resorption compared to teriparatide.
Supression of Sclerostin: Abaloparatide reduces screlostin expression in osteocytes which boosts Wnt/β-catenin signaling. This improves osteoblast proliferation, matrix synthesis and also bone formation itself while reducing inhibition of anabolic pathways.
Higher IGF-1 and VEGF Production: Abaloparatide increases the production of important pathways like IGF-1 and VEGF which are both crucial for bone growth purposes.
RANKL/OPG Modulation: Abaloparatide increases RANKL expression in osteoblasts which stimulates osteoclastogenesis, but because of its transient/temporary receptor binding and intermittent dosing the osteoblast driven bone formation overweights bone resorption. This shifts remodeling towards net anabolic gain with a lower risk profile compared to teriparatide.
Collagen Synthesis and Osteoblast Survival: Abaloparatide stimulates type I collagen synthesis in osteoblasts which provides the structural framework for mineral deposition which is important for bones. To add on cAMP/PKA signaling prolongs osteoblast lifespan by inhibiting apoptosis (programmed cell death) which also results in more sustained bone matrix production.
Reactivation of Quiescent Bone Lining Cells: Bone lining cells on quiescent surfaces can be reactivated or literally "woken up" by abaloparatide to resume matrix secretion and contribute to surface based bone formation. This increases the amount of active bone-forming cells and helps to reactivate them on previously inactive bone surfaces
Stimulation of MSC Differentiation: Abaloparatide promotes mesenchymal stem cell (MSC) differentiation toward the osteoblast lineage also
reduces adipogenesis in bone marrow and refreshing the osteoblast pool for long term bone formation capacity.
Enhanced Osteoblast Activity: Osteoblasts which are exposed to abaloparatide show increased synthesis of collagen, osteocalcin and alkaline phosphatase activity. All of which are very important for mineralization and robust bone matrix deposition.
Improved Osteocyte Function: Abaloparatide signaling reduces osteocyte apoptosis and suppresses sclerostin further which strenghtens the ability of osteocytes to sense strain and regulate remodeling.
Promotion of Chondrocyte Recruitment: Abaloparatide supports chondrocyte recruitment and differentiation during fracture and growth which enhances endochondral ossification. This accelerates callus formation, mineralization and fracture repair.
Cons
https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/208743Orig1s015lbl.pdf
Cortical Bone Caveate: Abaloparatide also mainly improves trabecular spongy bone especially in areas like the spine and pelvis, but in cortical compact bone (like in long bone shafts) abaloparatide can causes temporary porosity early in treatment caused by the increased bone turnover on the surface before new bone formation fills in. This is a temporary effect and will recover to normal once treatment is followed by an antiresorptive drug like a bisphosphonates or denosumab.
Losing Bone Gains: Pretty similar to teriparatide the benefits of abaloparatide can decline when therapy is stopped or completed. Bone mineral density (BMD) and bone gains during treatment decreases within 1-2 years and fracture protection will weaken as time goes on. To preserve the gains you need to get treated with an antiresorptive agent (for example bisphosphonates or denosumab) which basically helps to lock in the newly formed bone and maintain strength.
Study (1)
Common Side Effects
Hypercalcemia: Abaloparatide injections cause a slight and temporary rise in serum calcium levels in some patients. The increase usually peaks 4-6 hours after the injection and recovers to normal levels within 16-24 hours. This happens because abaloparatide increases calcium release from bone and enhances intestinal calcium absorption indirectly. The increase is usually pretty small, but in sensitive patients it can cause symptoms like fatigue, nausea, constipation or muscle weakness. Severe hypercalcemia is uncommon, but calcium levels should be monitored as some people respond bad.
Nausea: This is a common side effect of abaloparatide and occurres within the first few hours of injection. It is mild and temporary most of the time and the exact cause is not fully understood, but it is likely related to temporary shifts in calcium metabolism or sensitivity in the central nervous system to these changes.
Headache: Some patients report experiencing headaches particularly in the first few weeks of treatment. The headaches are usually mild to moderate and tend to resolve as the body adapts to daily injections. This could be due to changes in vascular tone or fluctuations in calcium and phosphate levels.
Muscle Cramping: This is also reported as a side effect of abaloparatide. This is likely related to altered calcium and electrolyte handling in muscle fibers, as calcium plays a critical role in muscle contraction and relaxation. The cramps are generally temporary and can be minimized with hydration.
Joint Pain: Some patients may experience mild joint pain during treatment with abaloparatide. This is due to increased bone turnover which can cause temporary stress in joints. This effect reflects the body's adjustment to active bone remodeling rather than any joint damage. The pain is typically manageable and resolves as treatment continues.
Fatigue: A feeling of tiredness or low energy is common early in therapy with abaloparatide. This fatigue is typically temporary and resolves as the body adapts to the increased metabolic activity caused by bone remodeling. Calcium and vitamin D intake may help reduce this side effect.
Rare Side Effects
Hyperuricemia: Abaloparatide increases uric acid levels in the blood through changes in mineral metabolism and kidney handling. The increase is pretty small but it can potentially trigger gout flares in patients with a history of gout or kidney stones. Extreme cases are uncommon but monitoring is recommended for people with higher risk.
Calciphylaxis: Another uncommon but serious side effect of abaloparatide is calciphylaxis which occures in patients with severe kidney disease or advanced vascular pathology. This condition causes calcium to deposit abnormally in small blood vessels of the skin and fat whichs leads to painful skin ulcers, necrosis and a risk of infection.
Hypercalciuria: Hypercalciuria (high calcium levels in the urine) occurs as a result of elevated blood calcium, which can predispose patients to kidney stones (nephrolithiasis). This risk is higher in people with a history of kidney stones or renal impairments. Its usually mild but monitoring urine calcium levels and ensuring enough hydration can help reduce this risk.
Orthostatic Hypotension: Some patients may experience lightheadedness or dizziness when standing up after the first few injections. This is caused by orthostatic hypotension which is a temporary drop in blood pressure that is likely caused by vasodilation from abaloparatide’s signaling effects. It only occures with the first few injections but it is recommended to inject in a seated position.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/208743Orig1s015lbl.pdf
Cortical Bone Caveate: Abaloparatide also mainly improves trabecular spongy bone especially in areas like the spine and pelvis, but in cortical compact bone (like in long bone shafts) abaloparatide can causes temporary porosity early in treatment caused by the increased bone turnover on the surface before new bone formation fills in. This is a temporary effect and will recover to normal once treatment is followed by an antiresorptive drug like a bisphosphonates or denosumab.
Losing Bone Gains: Pretty similar to teriparatide the benefits of abaloparatide can decline when therapy is stopped or completed. Bone mineral density (BMD) and bone gains during treatment decreases within 1-2 years and fracture protection will weaken as time goes on. To preserve the gains you need to get treated with an antiresorptive agent (for example bisphosphonates or denosumab) which basically helps to lock in the newly formed bone and maintain strength.
Study (1)
Common Side Effects
Hypercalcemia: Abaloparatide injections cause a slight and temporary rise in serum calcium levels in some patients. The increase usually peaks 4-6 hours after the injection and recovers to normal levels within 16-24 hours. This happens because abaloparatide increases calcium release from bone and enhances intestinal calcium absorption indirectly. The increase is usually pretty small, but in sensitive patients it can cause symptoms like fatigue, nausea, constipation or muscle weakness. Severe hypercalcemia is uncommon, but calcium levels should be monitored as some people respond bad.
Nausea: This is a common side effect of abaloparatide and occurres within the first few hours of injection. It is mild and temporary most of the time and the exact cause is not fully understood, but it is likely related to temporary shifts in calcium metabolism or sensitivity in the central nervous system to these changes.
Headache: Some patients report experiencing headaches particularly in the first few weeks of treatment. The headaches are usually mild to moderate and tend to resolve as the body adapts to daily injections. This could be due to changes in vascular tone or fluctuations in calcium and phosphate levels.
Muscle Cramping: This is also reported as a side effect of abaloparatide. This is likely related to altered calcium and electrolyte handling in muscle fibers, as calcium plays a critical role in muscle contraction and relaxation. The cramps are generally temporary and can be minimized with hydration.
Joint Pain: Some patients may experience mild joint pain during treatment with abaloparatide. This is due to increased bone turnover which can cause temporary stress in joints. This effect reflects the body's adjustment to active bone remodeling rather than any joint damage. The pain is typically manageable and resolves as treatment continues.
Fatigue: A feeling of tiredness or low energy is common early in therapy with abaloparatide. This fatigue is typically temporary and resolves as the body adapts to the increased metabolic activity caused by bone remodeling. Calcium and vitamin D intake may help reduce this side effect.
Rare Side Effects
Hyperuricemia: Abaloparatide increases uric acid levels in the blood through changes in mineral metabolism and kidney handling. The increase is pretty small but it can potentially trigger gout flares in patients with a history of gout or kidney stones. Extreme cases are uncommon but monitoring is recommended for people with higher risk.
Calciphylaxis: Another uncommon but serious side effect of abaloparatide is calciphylaxis which occures in patients with severe kidney disease or advanced vascular pathology. This condition causes calcium to deposit abnormally in small blood vessels of the skin and fat whichs leads to painful skin ulcers, necrosis and a risk of infection.
Hypercalciuria: Hypercalciuria (high calcium levels in the urine) occurs as a result of elevated blood calcium, which can predispose patients to kidney stones (nephrolithiasis). This risk is higher in people with a history of kidney stones or renal impairments. Its usually mild but monitoring urine calcium levels and ensuring enough hydration can help reduce this risk.
Orthostatic Hypotension: Some patients may experience lightheadedness or dizziness when standing up after the first few injections. This is caused by orthostatic hypotension which is a temporary drop in blood pressure that is likely caused by vasodilation from abaloparatide’s signaling effects. It only occures with the first few injections but it is recommended to inject in a seated position.

Recombinant Full-Length PTH
I will not be explaining this one in-depth as teriparatide and abaloparatide are superior for bone building. The reason for the 1-34 PTH analogues being superior is because they are far more studied with more data, the actual "anabolic" part is the N-terminal so adding the C-terminal hasn't shown a clinical anabolic advantage over the N-terminal alone. To add on, recombinant full-length PTH analogue 1-84 is only approved for hypoparathyroidism by FDA and not something like osteoporosis. Getting the PTH analogue itself is a pain in the ass too as the producers of Natpara (Recombinant Full-Length PTH Analogue) have announced that they globally discontinued its manufacturing. There is also no evidence for it being safer or "better" in any way.
Usages
As I've said PTH analogue's main clinical use is on women with high fracture risk, postmenopausal women and women/men with osteoporosis, its uses for anything else isn't heavily studied so its mostly theoretical and the risks are up to you although i wouldn't advise its usage and surely don't ever touch it if you aren't familiar with the compound or any compound at all. My own use for teriparatide is its particular effects on bone tissue and bone-building cells which is perfectly what I'm looking for. In theory this compound will help bone remodeling and any healing process that's for sure but it's effects on bone growth by itself should moderate or at the least minimal but trying doesn't hurt, also my reasoning is because of teriparatide's cellular/molecular pros. It should also potentially synergise well with other peptides and steroids used in a usual "heightmaxxing" stack, so i see potential in PTH analogues and will use them myself.

Dosages
The dosages vary for the main PTH analogues but the clinical approved ones and the doses used on most patients are; 20µg for teriparatide, 80µg for abaloparatide and 100µg for recombinant full-length PTH. This doesn't mean that going above any of these doses is lethal or that their effects become diminishing it actually becomes even more potent most of the time and you can still keep a positive remodeling balance without it tipping into bone loss, although it isn't recommended as it carries even more risks and the rare side effects become much more realistic and probable.
For teriparatide for example , this means that as the doses increase it becomes even more potent but after a certain point which is the "anabolic window" if the exposure is too high or too continous (not intermittently dosed) bone resorption overweights bone formation and it results in net bone loss, so its either "anabolic" or "catabolic". While the usual 20µg dose is very potent itself you can always increase the dose to an amount like 40µg which makes the pros even more significant but it comes with more of the common adverse effects that I've explained in the thread, but it still keeps you in that "anabolic" state. Some countries like Japan use once-weekly injections of 56.5µg teriparatide instead of the daily injections. At last i would suggest you use 20µg instead of the higher doses at the beginning and if you know what you're doing and respond well then you can think about upping the dose up to 40µg.
For abaloparatide it has also been shown that it exhibits dose-dependent anabolic effects on bone, that means as the dose increases it becomes even more potent just like teriparatide. The way abaloparatide binds to the PTH1 receptors favoring the RG conformation means it produces shorter and more temporary bursts of signaling. It's bias allows it to become even more potent than teriparatide but still have less adverse effects and less drive towards bone resorption. The usual and approved dose is 80µg daily which led to very rapid and significant gains in clinical trials, although lower doses like 40µg were also studied it did give improvements on bone but of course the 80µg dose was far superior without many sides added. Doses above 80µg haven't been studied yet as abaloparatide already exhibits a strong anabolic response with minimal side effect profile but in theory it should be safer to dose abaloparatide higher cause of it's conformation bias.

Costs & Sourcing
The costs largely depend on where you're getting it from but aren't unrealistic if we choose a Chinese manufacturer which provides the raw powder of the compound which you then have to put in vials yourself, another choice you have is getting it in vials but the costs do rise in that case. The best choice is getting it from a research institution as that will almost fully guarantee sterility and purity but they require proof of you being an actual researcher or that you own a research institution yourself. One source that is quite publicly known around the forum is Indiamart, you can also find some of the PTH analogues there like teriparatide although the prices are moderate the safety isn't guaranteed as you're buying it from an almost random vendor but it is pharmaceutical grade (Teriparatide Link). As you can see 600 mcg of teriparatide costs 25,000 Rupees which converts to around €250/$290/£210 for a 30 day supply of teriparatide.
Look around for other vendors and find the best one that suits your budget but be sure to check the seller's reviews and "rank" on the site itself. Another thing you should look out for is if the compound will actually get delivered and not seized as some countries are strict with customs, check your country's law and ask the seller himself. For me any shipment directly from India to the Netherlands gets seized instantly, what you can do is ask the seller for any other shipping method and one that ships to another EU country first to ensure the shipping is from another EU country to your own homeland that way the shipping is almost guaranteed to be received by you. You can also do your own research and find a seller yourself but be mindful and don't get yourself scammed in the end and watch out for some of the dropshippers.
Thank you for reading (if you even have read this monstrosity) this took me a long amount of time as i had to learn all this myself and as i learnt more i had to update the thread, but now i will be working on my next thread which will be on HDACi and i hope this thread has helped you in any way.
Tags: @menas @Sadist @chadisbeingmade @SlayerJonas @Bitchwhipper2
Last edited: