E
el hit
true kshatriya
- Joined
- Sep 4, 2025
- Posts
- 631
- Reputation
- 995
to understand the drug, we first must understand sclerostin. our bones are not static they are constantly being remodeled in a balanced cycle where old, damaged bone is broken down and replaced by new bone. this process is orchestrated by two teams of specialized cells: osteoclasts and osteoblasts.
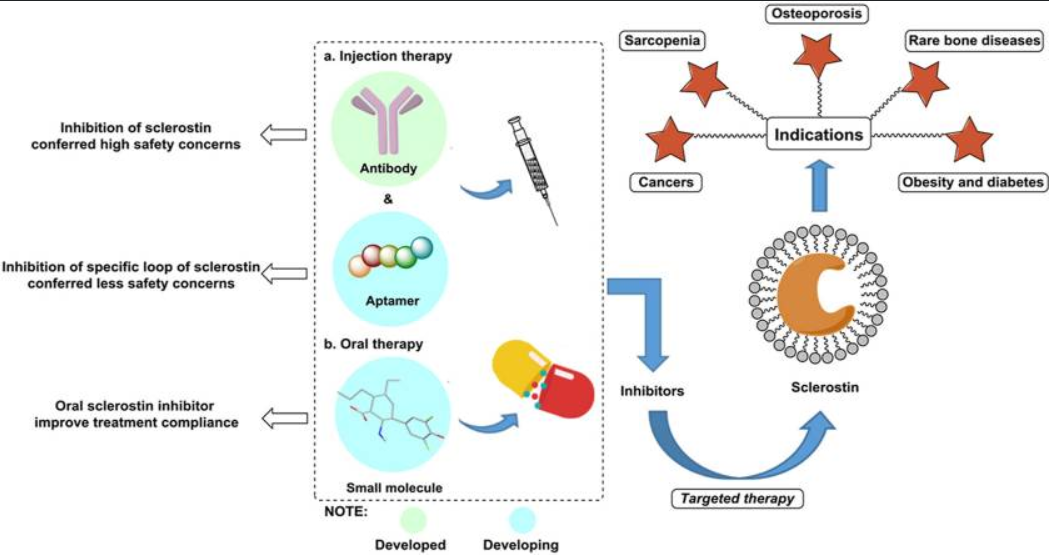
the protein sclerostin is produced mainly by bone cells called osteocytes. its primary function is to act as a negative regulator, a built-in emergency brake on bone growth. when the body senses that enough bone has been built, or perhaps needs to conserve resources, sclerostin is released. it works by interfering with one of the most fundamental processes for cell growth and division in the body: the wnt signaling pathway. sclerostin physically attaches itself to specific receptor proteins on the surface of the bone building cells, namely the LRP5 and LRP6 co receptors. By binding there, it blocks the necessary wnt signals from getting through. This effectively shuts down the osteoblast construction crew, dramatically reducing the rate of bone formation. compounding the problem, the suppression of osteoblasts indirectly encourages the activity of the bone-resorbing osteoclasts. In conditions like postmenopausal osteoporosis, the balance is heavily tipped because the body produces too much sclerostin, causing the builders to stand idle while the demolishers run rampant, resulting in rapid bone loss and fracture risk.
the scientific breakthrough was the creation of a drug, romosozumab, designed to neutralize sclerostin. romosozumab is classified as a monoclonal antibody. A monoclonal antibody is a laboratory made protein that has been meticulously engineered to be a perfect molecular match for only one target, in this case, sclerostin. when administered, it circulates through the body, finds the free-floating sclerostin proteins, and binds tightly to them. This act of binding neutralizes the sclerostin, preventing it from ever reaching the LRP5/6 receptors on the bone-forming cells.
by blocking the sclerostin, the brake is lifted, and the wnt signaling pathway is turned back on. This sends a massive, powerful signal to the ssteoblasts, causing them to rush into action and accelerate bone formation at an unprecedented rate. This is the drug’s greatest advantage is that it provides a unique dual effect. It is anabolic while simultaneously being anti resorptive. This dual capacity allows it to achieve significant and rapid gains in bone mineral density. Clinical trials, such as the FRAME and ARCH studies, confirmed this, showing that romosozumab significantly reduced the risk of both new vertebral and nonvertebral fractures in women with severe osteoporosis.
 pmc.ncbi.nlm.nih.gov
tldr
pmc.ncbi.nlm.nih.gov
tldr
the drug romosozumab works by disabling the protein sclerostin, which is your bodys natural brake on bone formation. by binding to sclerostin, the drug lifts the brake, activating your bone-building cells to rapidly build new bone mass while simultaneously slowing bone breakdown.
hope it helps, rep if you like it.
let me know if you have any questions
the protein sclerostin is produced mainly by bone cells called osteocytes. its primary function is to act as a negative regulator, a built-in emergency brake on bone growth. when the body senses that enough bone has been built, or perhaps needs to conserve resources, sclerostin is released. it works by interfering with one of the most fundamental processes for cell growth and division in the body: the wnt signaling pathway. sclerostin physically attaches itself to specific receptor proteins on the surface of the bone building cells, namely the LRP5 and LRP6 co receptors. By binding there, it blocks the necessary wnt signals from getting through. This effectively shuts down the osteoblast construction crew, dramatically reducing the rate of bone formation. compounding the problem, the suppression of osteoblasts indirectly encourages the activity of the bone-resorbing osteoclasts. In conditions like postmenopausal osteoporosis, the balance is heavily tipped because the body produces too much sclerostin, causing the builders to stand idle while the demolishers run rampant, resulting in rapid bone loss and fracture risk.
the scientific breakthrough was the creation of a drug, romosozumab, designed to neutralize sclerostin. romosozumab is classified as a monoclonal antibody. A monoclonal antibody is a laboratory made protein that has been meticulously engineered to be a perfect molecular match for only one target, in this case, sclerostin. when administered, it circulates through the body, finds the free-floating sclerostin proteins, and binds tightly to them. This act of binding neutralizes the sclerostin, preventing it from ever reaching the LRP5/6 receptors on the bone-forming cells.
by blocking the sclerostin, the brake is lifted, and the wnt signaling pathway is turned back on. This sends a massive, powerful signal to the ssteoblasts, causing them to rush into action and accelerate bone formation at an unprecedented rate. This is the drug’s greatest advantage is that it provides a unique dual effect. It is anabolic while simultaneously being anti resorptive. This dual capacity allows it to achieve significant and rapid gains in bone mineral density. Clinical trials, such as the FRAME and ARCH studies, confirmed this, showing that romosozumab significantly reduced the risk of both new vertebral and nonvertebral fractures in women with severe osteoporosis.
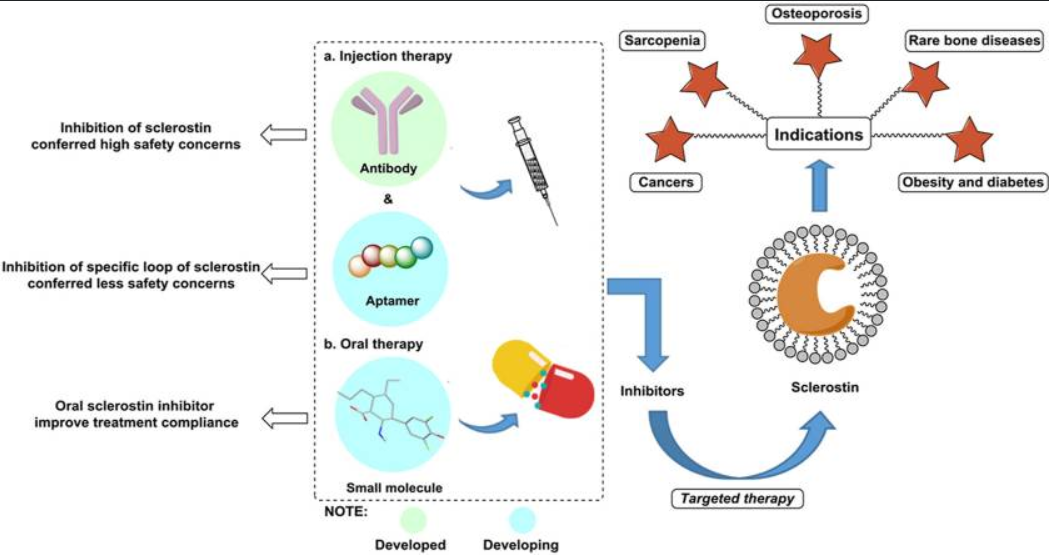
Table - PMC
Sclerostin, a protein secreted from osteocytes, negatively regulates the WNT signaling pathway by binding to the LRP5/6 co-receptors and further inhibits bone formation and promotes bone resorption. Sclerostin contributes to musculoskeletal ...
the drug romosozumab works by disabling the protein sclerostin, which is your bodys natural brake on bone formation. by binding to sclerostin, the drug lifts the brake, activating your bone-building cells to rapidly build new bone mass while simultaneously slowing bone breakdown.
hope it helps, rep if you like it.
let me know if you have any questions
Last edited:



