nvr13
nvr13
- Joined
- May 15, 2025
- Posts
- 125
- Reputation
- 131
Hello buddy boyos, some of you guys may know me from the org cord; but I have some stuff to share with the site 
I present to you all:
FULL THREAD GUIDE TO LARPING AN AHI INDEX

So why would you want to fake this? muhh what is a AHI score?
AHI is short for Apnea-Hypopnea Index, which is typically used to measure sleep apnea. This is commonly used for sleep study test to measure the severity of OSA (Obstructive Sleep Apnea).
This is done through a polysomnography test, which is either monitored nasally or orally (typically nasally).
Polysomnography tests (sleep study) are an overnight exam that records body functions during sleep. small sensors are placed on your scalp, face, chest, and legs to measure brain waves (EEG), eye movements, muscle activity, heart rhythm, and breathing. airflow is tracked through nasal prongs, tubes, or oral sensors, while belts around the chest and abdomen measure effort of inhalation. oxygen levels are checked with a finger probe. the test is painless, done in a sleep lab, and provides detailed data to calculate the ahi score.
Now why exactly would you want to fake this index? Seems pointless; sleeping better is ideal for growth is it not?
one word:
Surgery.
Im going to list THEORETICAL AND REASEARCH HELPING to increasing your AHI Index score on a polysomnography.
<<AFTER YOU ARE DONE READING THIS, READ THE END OF THE THREAD FOR INFO AND SCORING.>>
This is the first and most recommended method, also impossible to get caught by your provider; since sleeping on your back is already a chronic sleep apnea sufferers' profile for sleep. <<ALSO ATTEMPT TO MAKE YOUR MANDIBLE PUSHED BACK OR TUCKED TO INDUCE MOUTHBREATHING>>
This method is possibly detectable/noticeable if being tested by an experienced polysomnographic tester. It is recommended to micro dose the Lidocaine or other topical numbing agents with doses of about <1mg.
This is also another strongly reccomended method, as they cant just deny a tired person jfl 

can possibly increase AHI by 7 points if done correctly
This is the least recommended, but most potent and efficient. Could possibly put you in hypoxic state if done too strong, but it is highly unlikely you will get hurt if you're being monitored by people who are responsible for checking your sleep. Micro dosing is recommended, of about 2.75g (Incrementally higher than therapeutic, medical reasons.) <<ALCOHOL IS ALSO A POSSIBLE OPTION, BUT IS NOT RECCOMENDED, AS IT CAN CAUSE A WIDE MARGIN FOR DIFFERENCE IN AHI GRAPHS.
Strongly recommended, and would inherently contribute to your AHI Index about 5-6 points if induced properly, and paired with several other methods.
Now that we have covered the methods, I will now go over some proper notes before I conclude this thread.
1. Understanding the AHI Index
2. Effects on AHI through pharmacological and/or systemic manipulation
Induced sleep deprivation
– Can raise AHI by 10–15/hr
– May shift normal → mild or mild → moderate
Back sleeping (supine)
– Often doubles baseline AHI
– Mild → moderate or moderate → severe
Chin tuck
– Adds 5–10/hr
– Can move mild → moderate
Brainstem depressants
– Raises AHI 5–15/hr
– Mild → moderate or moderate → severe
Induced nasal congestion
– Raises AHI 3–7/hr
– Usually not enough to change category alone
Topical numbing agents
– Small, short-lived increase (1–5/hr)
– Rarely changes severity class
3. Most efficient methods of pairing
Most effective (hardest to distinguish from natural variation)
Concluding notes
Keep in mind that this is not guaranteed to work, and the possibility of you getting caught still exists (exponentially low, basically ~<3%)
Now its really just a matter of scoring high enough with your AHI test. You can try these methods yourself at home before trying them at an actual sleep study clinic; and see which ones work the best accordingly.
Make sure to put on a good front to a certain group of people (use context clues now, its a separate group from the polysomnographic doctors) about TMJ, trouble chewing, breathing, etc.
Try jutting your mandible back minorly to appear recessed/more recessed (if your reading this, you're probably recessed jfl), speak with an ever so slightly lisp and try to correct yourself a few times on occasion, complain about chronic jaw pain, facia system issues (facial muscles, typically strained from improper skeletal to muscular tension loads)
If all goes well, you may be able to get surgical compensation, IN THEORY
Thanks for reading my research-use only guide bhais
I present to you all:
FULL THREAD GUIDE TO LARPING AN AHI INDEX

So why would you want to fake this? muhh what is a AHI score?
AHI is short for Apnea-Hypopnea Index, which is typically used to measure sleep apnea. This is commonly used for sleep study test to measure the severity of OSA (Obstructive Sleep Apnea).
This is done through a polysomnography test, which is either monitored nasally or orally (typically nasally).
Polysomnography tests (sleep study) are an overnight exam that records body functions during sleep. small sensors are placed on your scalp, face, chest, and legs to measure brain waves (EEG), eye movements, muscle activity, heart rhythm, and breathing. airflow is tracked through nasal prongs, tubes, or oral sensors, while belts around the chest and abdomen measure effort of inhalation. oxygen levels are checked with a finger probe. the test is painless, done in a sleep lab, and provides detailed data to calculate the ahi score.
Now why exactly would you want to fake this index? Seems pointless; sleeping better is ideal for growth is it not?
one word:
Surgery.
Im going to list THEORETICAL AND REASEARCH HELPING to increasing your AHI Index score on a polysomnography.
<<AFTER YOU ARE DONE READING THIS, READ THE END OF THE THREAD FOR INFO AND SCORING.>>
One of the most effective and least suspicious methods is in fact one of the most simple. This is due to the throat collapse of back sleeping. For those of you who may or may not already have issues, then effectiveness will vary for each person.

This diagram shows and demonstrates the palatal collapse caused by OSA. For any user, AHI has been proven to increase the most from back sleeping, due to the risk of temporary airway collapse being determined heavily by your position
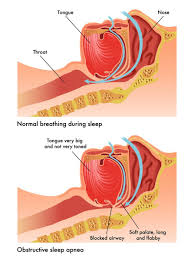
This diagram shows and demonstrates the palatal collapse caused by OSA. For any user, AHI has been proven to increase the most from back sleeping, due to the risk of temporary airway collapse being determined heavily by your position
This is the first and most recommended method, also impossible to get caught by your provider; since sleeping on your back is already a chronic sleep apnea sufferers' profile for sleep. <<ALSO ATTEMPT TO MAKE YOUR MANDIBLE PUSHED BACK OR TUCKED TO INDUCE MOUTHBREATHING>>
Local anesthetics like lidocaine temporarily reduce sensation in muscle in the upper airway. Reflexes in the throat and pharynx help keep the airway open during sleep; tiny sensory inputs trigger slight muscle contractions that tighten and contract the airway walls. If you blunt those reflexes, the airway is more prone to collapse under negative pressure while breathing in, especially in REM or back-sleeping. That leads to more frequent apneas and hypopneas, which mathematically increases the AHI.
Additionally, numbing the throat can disrupt the normal arousal response. In untreated sleep apnea, partial collapses usually trigger micro-arousals that restore tone and reopen the airway. With dampened sensation, the collapses may last longer or occur more often before the body compensates, raising the recorded AHI score. This effect has actually been observed in research studies where topical anesthetics were used to probe the role of airway reflexes in sleep-disordered breathing.

Additionally, numbing the throat can disrupt the normal arousal response. In untreated sleep apnea, partial collapses usually trigger micro-arousals that restore tone and reopen the airway. With dampened sensation, the collapses may last longer or occur more often before the body compensates, raising the recorded AHI score. This effect has actually been observed in research studies where topical anesthetics were used to probe the role of airway reflexes in sleep-disordered breathing.

Sleep deprivation actually plays a major role in how your airway behaves during a sleep study. When you’re severely deprived of sleep, your brain spends more time in REM rebound once you finally do rest. REM sleep is the stage where your body loses the most muscle tone, including the pharyngeal dilator muscles that normally help keep the throat open. Less tone = more frequent airway collapses.
On top of that, being overtired raises your arousal threshold. In other words, your brain is slower to wake you up when your breathing is obstructed. Instead of a quick gasp or micro-arousal ending a partial collapse, the airway can remain blocked for longer, which increases both the length and number of apneas and hypopneas. This can make the calculated AHI appear higher, because the index reflects both frequency and duration of these events.
On top of that, being overtired raises your arousal threshold. In other words, your brain is slower to wake you up when your breathing is obstructed. Instead of a quick gasp or micro-arousal ending a partial collapse, the airway can remain blocked for longer, which increases both the length and number of apneas and hypopneas. This can make the calculated AHI appear higher, because the index reflects both frequency and duration of these events.
can possibly increase AHI by 7 points if done correctly
Brainstem depressants can also make AHI scores go up. These substances slow down the nervous system and weaken the signals that normally keep the throat muscles active during sleep. With less tone in the upper airway, it’s much easier for the airway to collapse.
They also blunt the arousal response. Normally, if your breathing stops, the brainstem quickly kicks you into a lighter stage of sleep so the airway reopens. Depressants dull this reflex, meaning apneas can last longer and happen more often before you wake up. The result is an inflated AHI score because both the frequency and duration of events increase.


They also blunt the arousal response. Normally, if your breathing stops, the brainstem quickly kicks you into a lighter stage of sleep so the airway reopens. Depressants dull this reflex, meaning apneas can last longer and happen more often before you wake up. The result is an inflated AHI score because both the frequency and duration of events increase.
This one is kind of self-explanatory. Clogging or congesting your nasal cavity/passageway can induce mouth breathing for sleep apnea studies. (obvious)
Here are methods ranked G ----> L to induce monitored congestion.

Here are methods ranked G ----> L to induce monitored congestion.
- standardized allergen challenge (pollen, dust mite, etc.)
- topical histamine spray
- topical bradykinin / leukotriene application
- chemical irritants (capsaicin, acetic acid vapor, smoke exposure)
- viral infection models (e.g., rhinovirus inoculation)
- cold dry air provocation
- hypertonic saline spray / irrigation
- simple physical factors (supine posture, head-down tilt increasing nasal venous engorgement)
Strongly recommended, and would inherently contribute to your AHI Index about 5-6 points if induced properly, and paired with several other methods.
Now that we have covered the methods, I will now go over some proper notes before I conclude this thread.
1. Understanding the AHI Index
AHI Scoring
- Normal: <5/hr
- Mild OSA: 5–14/hr
- Moderate OSA: 15–29/hr
- Severe OSA: ≥30/hr
2. Effects on AHI through pharmacological and/or systemic manipulation
Induced sleep deprivation
– Can raise AHI by 10–15/hr
– May shift normal → mild or mild → moderate
Back sleeping (supine)
– Often doubles baseline AHI
– Mild → moderate or moderate → severe
Chin tuck
– Adds 5–10/hr
– Can move mild → moderate
Brainstem depressants
– Raises AHI 5–15/hr
– Mild → moderate or moderate → severe
Induced nasal congestion
– Raises AHI 3–7/hr
– Usually not enough to change category alone
Topical numbing agents
– Small, short-lived increase (1–5/hr)
– Rarely changes severity class
3. Most efficient methods of pairing
Most effective (hardest to distinguish from natural variation)
- Sleep deprivation (REM rebound)
- Back sleeping (supine)
- Chin tuck (neck flexion)
+ Induced nasal congestion
- Brainstem depressants (alcohol, sedatives, GHB, etc.)
- Topical numbing agents
- Equipment tampering (cannula, oximetry, don't even try this jfl, youll get ur sleep study cancelled
- Exaggerated symptom reporting
Concluding notes
Keep in mind that this is not guaranteed to work, and the possibility of you getting caught still exists (exponentially low, basically ~<3%)
Now its really just a matter of scoring high enough with your AHI test. You can try these methods yourself at home before trying them at an actual sleep study clinic; and see which ones work the best accordingly.
Make sure to put on a good front to a certain group of people (use context clues now, its a separate group from the polysomnographic doctors) about TMJ, trouble chewing, breathing, etc.
Try jutting your mandible back minorly to appear recessed/more recessed (if your reading this, you're probably recessed jfl), speak with an ever so slightly lisp and try to correct yourself a few times on occasion, complain about chronic jaw pain, facia system issues (facial muscles, typically strained from improper skeletal to muscular tension loads)
If all goes well, you may be able to get surgical compensation, IN THEORY
Thanks for reading my research-use only guide bhais


 , i wake up tired, i never sleep good, i snore, and all this but i never wake up or stop breathing.
, i wake up tired, i never sleep good, i snore, and all this but i never wake up or stop breathing.
 living in a poor country, life is JFL
living in a poor country, life is JFL