Nexom


Alea iacta est
- Joined
- Jan 15, 2022
- Posts
- 2,475
- Reputation
- 3,861
DISCLAIMER
This is NOT a guide or a request for a diagnosis. I know you guys aren't doctors and I'm not expecting a diagnosis or a miracle solution. It's an open discussion on this topic with my specific situation as a starting point, where people can look back and find anything of value in the thread, even if it means just 2 replies. I'm just trying to find out to what extent this marker translates into looks.
I'm posting this because I feel like either this topic isn't talked about enough, I've somehow missed the obvious, the answer is something braindead/simple that I haven't figured out, or I'm just a weird outlier case. If you're gonna troll, just skip the thread. But if you can take it seriously then feel free to chime in with anything you've got, literally.
I'm posting this because I feel like either this topic isn't talked about enough, I've somehow missed the obvious, the answer is something braindead/simple that I haven't figured out, or I'm just a weird outlier case. If you're gonna troll, just skip the thread. But if you can take it seriously then feel free to chime in with anything you've got, literally.
I was recently browsing some older threads and found a post by @Orc showing a biomarker trajectory graph from the study Quantification of biological aging in young adults and something in there piqued my interest. I've noticed that inflammation markers (like hsCRP in this cohort) show up a lot in biological aging models. In the same line of research, people with high chronic inflammation are literally rated as looking older, with puffier faces and inflammed appearance.
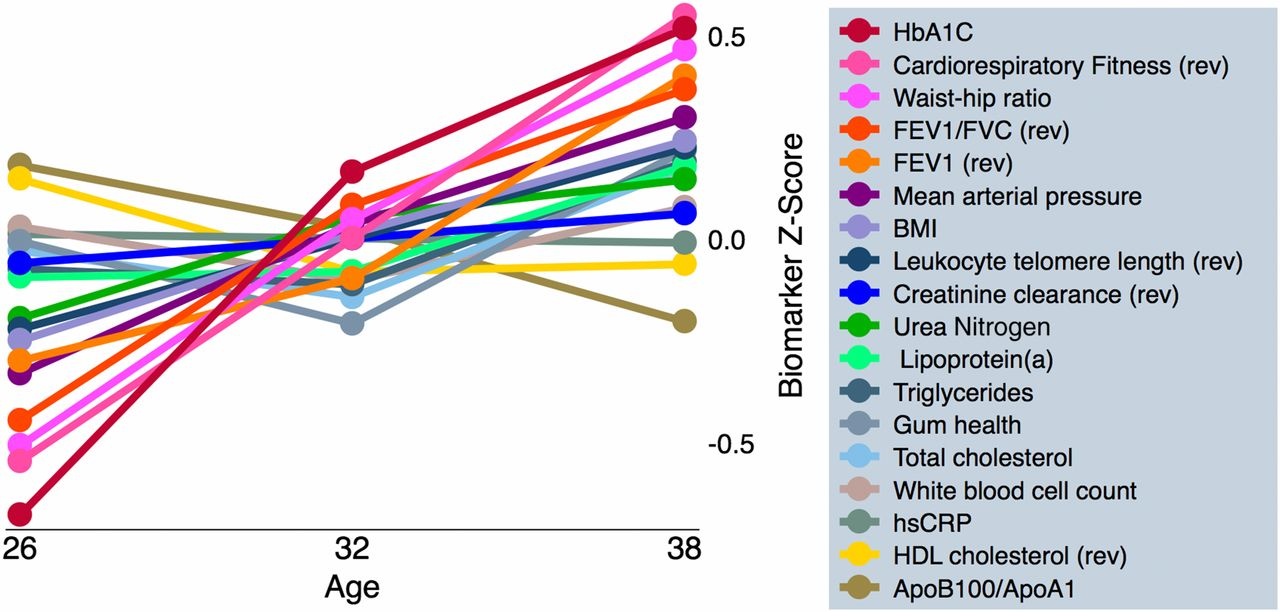
Even if hsCRP looks irrelevant compared to the other lines in the graph, I've been trying to get some clarity on the hsCRP <=> looks relationship for some time. I've been having a more health = looks approach recently instead of treating them separately. Most people know health is looks, but as we age we realise it's more important than we thought. In this thread I'm mostly presenting my situation as a starter, and opening a dialogue on hsCRP + looks while also creating a future reference people can search later on.
MAIN ISSUE
My hsCRP is elevated, but my CRP is within the reference range and basically everything else looks acceptable (full labs at the bottom).
I've taken many measurements of hsCRP/CRP about 2 weeks apart under stable conditions throughout the past years and they've always hovered around the most recent results below.
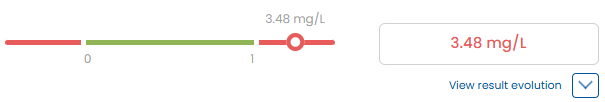
hsCRP: 3.48mg/L

This is a high value, and within the"high-risk" range of >3 (Source)
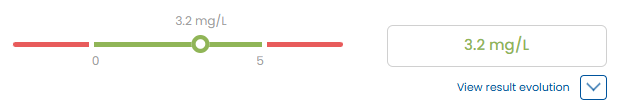
CRP: 3.2mg/L (ref 0-5 so "normal")
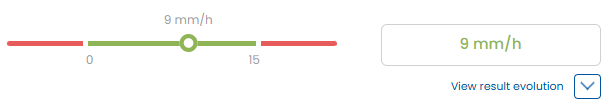
ESR: normal
CBC: normal
Autoimmune markers: negative
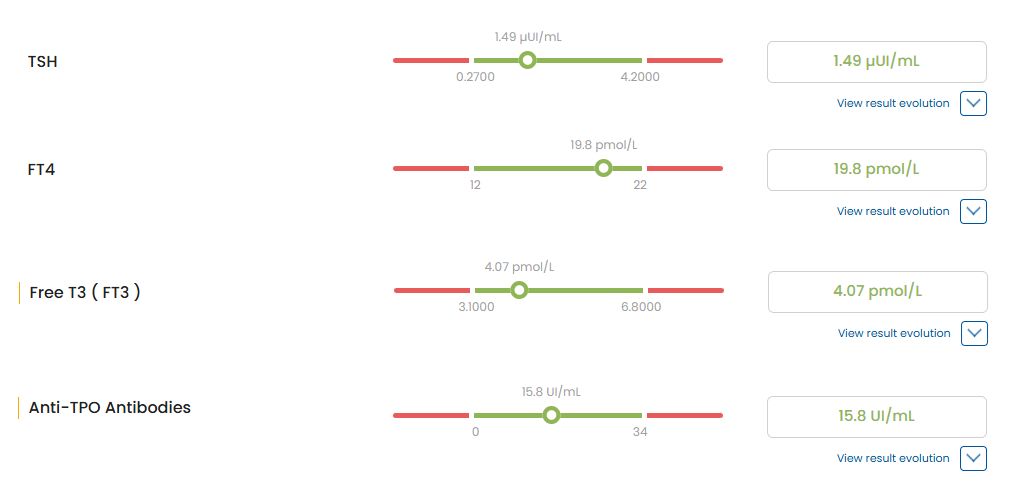
Glucose/insulin/lipids/thyroid/liver/kidney: mostly good
Note: hsCRP and CRP basically measure the same protein.
The difference is hsCRP is a more sensitive assay used to interpret low-grade baseline inflammation.
My CRP isn't high as in acute inflammation, but sits around 3mg/L consistently which is considered high if you interpret it as hsCRP/low-grade inflammation.

Why this matters for looks?
Keeping inflammation low is relatively underrated for looks, and ironically seems to be pretty foundational. It goes without saying that high inflammation means skin quality issues, redness, collagen issues, puffiness, destroys the under-eye area, gives an "inflammed" face, not to mention the myriad of indirect issues it causes. No, it won't fix your canthal tilt or maxilla.
Chronic low-grade inflammation = “inflammaging” signals, and over time those signals can push collagen/skin structure in the wrong direction (partly via enzymes like MMPs that break down collagen).
There is also some human data pointing that way: in one study, women who were perceived as looking older tended to have higher BMI and higher hsCRP.
There's also the idea of inflammatory scalp conditions like seb derm, psoriasis, etc. as well as telogen effluvium shedding caused by high inflammation, although this is simply because of the dirsuption of the hair growth cycle (but it's not really a driver of androgenic alopecia as far as I'm aware). Hair requires an entirely different thread.
That being said, hsCRP is not correlated 1:1 to looking old by any means, especially because evidence is mixed, and at least one paper concludes that facial appearance was only weakly related to hsCRP.
Some context to eliminate the basics
Just to clarify, I've looked into my specific case throughout the years: I've read surface-level explanations, anecdotes, research papers, visited a few doctors and recently just searched probably this entire forum as well. Sometimes the simplest answer turns out to be the dumbest thing that hasn't been considered so I'm still open to that. Of course, I'm still gonna see a few more professionals about this.
• Diet: not plant-based, mostly whole foods. I don't eat vegetables mainly because I don't like their taste, not because I find them inherently evil or anything like that. I do fully cover my micronutrients almost at all times.
My diet is basically: all kinds of meat, animal organs, fish, eggs, sometimes dairy, lots of fruits, some sourdough, etc.
• Supplements: cut off all supplements about a year ago to eliminate variables, occasionally used some but not during testing periods.
• Sleep: Prior to the bloodwork below, my sleep was very consistent and sufficient.
I have a slightly deviated septum but haven't noticed it affect my sleep so far.
• Weight: I'm not overweight and haven't had a lot of visceral fat.
• Exercise: I didn't train before the hsCRP/CRP blood draw, so we can exclude "post-workout inflammation".
• Allergies: no known allergies, but I haven't done any allergy tests.
• Smoking: I rarely smoke cigarettes, but I use a few low to medium strength pouches throughout the day.
• PEDs: For full transparency, I did a single simple test cycle almost 10 years ago and haven't touched anything since. So if inflammation is happening, it's not because I'm on any sort of gear. It would be pretty pointless to think about this if I was on gear (?)
• Imaging: multiple CT scans of most of my body and nothing came up.
Just to clarify, I've looked into my specific case throughout the years: I've read surface-level explanations, anecdotes, research papers, visited a few doctors and recently just searched probably this entire forum as well. Sometimes the simplest answer turns out to be the dumbest thing that hasn't been considered so I'm still open to that. Of course, I'm still gonna see a few more professionals about this.
• Diet: not plant-based, mostly whole foods. I don't eat vegetables mainly because I don't like their taste, not because I find them inherently evil or anything like that. I do fully cover my micronutrients almost at all times.
My diet is basically: all kinds of meat, animal organs, fish, eggs, sometimes dairy, lots of fruits, some sourdough, etc.
• Supplements: cut off all supplements about a year ago to eliminate variables, occasionally used some but not during testing periods.
• Sleep: Prior to the bloodwork below, my sleep was very consistent and sufficient.
I have a slightly deviated septum but haven't noticed it affect my sleep so far.
• Weight: I'm not overweight and haven't had a lot of visceral fat.
• Exercise: I didn't train before the hsCRP/CRP blood draw, so we can exclude "post-workout inflammation".
• Allergies: no known allergies, but I haven't done any allergy tests.
• Smoking: I rarely smoke cigarettes, but I use a few low to medium strength pouches throughout the day.
• PEDs: For full transparency, I did a single simple test cycle almost 10 years ago and haven't touched anything since. So if inflammation is happening, it's not because I'm on any sort of gear. It would be pretty pointless to think about this if I was on gear (?)
• Imaging: multiple CT scans of most of my body and nothing came up.

What I'm actually trying to figure out
I'm aware that there are substances, pharma or peptides that could probably lower inflammation on paper.
I'm less interested in "patching" the marker and more interested in questions like:
- Is there an underlying cause to fix or cure?
- Is this one of those things that can be normal for some?
- How many of us have high hsCRP and just never test it?

Are meds the solution?
To be honest, I've been hesitant to use strong anti-inflammatory drugs just to force the hsCRP down, because it felt like masking something potentially fixable (if there even is an issue to begin with).
Example: I've seen Rinvoq (upadacitinib) mentioned (I see you @User28823) and other anti-inflammatory meds and I know I could probably crush inflammatory markers because it's literally a JAK inhibitor used for autoimmune/inflammatory diseases but I'm not trying to nuke my immune system and risk the side effects without actually at least knowing if I can find out the cause of this.

Another relevant idea: Genetics
@Chintuck22 posted a thread basically saying polymorphisms in the CRP gene can shift your baseline CRP and how much it spikes after exercise. That means some people just naturally sit at higher CRP or experience a slower recovery. I consider that a possibility, and it might just be genetically high baseline inflammation even if everything else looks normal. That being said, I'm not really happy with this being the case so I'm looking for further ideas.
Could it be a gut/fiber issue?
This could be cope or the actual answer. Since I don't eat vegetables, my fiber intake is likely lower than average. I've seen decent arguments that fiber changes the microbiome and increases SCFA-producing bacteria (butyrate, etc) which lowers inflammation. There's also a review specifically on fiber > microbiome > inflammatory diseases. This opens the door to the idea of low fiber > lower microbiome diversity > higher baseline inflammation even though my macros and micros look good. The only issue with this theory is I've felt my best while I did a year of strict carnivore, and I've also never really had any gut issues in my entire life. I'm aware that doesn't necessarily mean no gut inflammation though.
Other possible causes
There are a few more hidden candidates that compete for the cause of high hsCRP and often show up in literature.
• Dental inflammation: periodontitis has been associated with high hsCRP levels.
Solution: Go get a periodontal check, including gums, pockets, bleeding.
• Sleep apnea: even if we sleep enough, we may have sleep apnea and meta-analyses show high CRP/hsCRP in obstructive sleep apnea.
Solution: Either a home sleep apnea test or an actual sleep study to rule out.
• Helicobacter pylori: it's a stomach bacteria that can chronic gastritis sometimes with barely any symptoms.
Solution: A simple breath or stool test to check for it.
• Stress: can worsen sleep, recovery from physical exercise, etc. which all lead to higher inflammation.
Solution: Difficult to diagnose through bloods, cortisol/ACTH isn't enough to rule it out.
Could be diagnosed through sleep study, HR/HRV/BP.
• Chronic sinus or nasal inflammation: this can be low-grade inflammatory for years.
Solution: Go to the ENT and/or nasal exam/imaging.
Some questions for public knowledge
- Has anyone had hsCRP >3 with normal CRP for an extended period of time, and clean labs otherwise?
- If low inflammation is an underrated looksmax, what are some "not so obvious" things that keep people above that?
- What are some other braindead causes we might be missing?
BLOODWORK
I've done lots of blood draws throughout my life, but I've done this extensive round of bloods a while ago specifically for two reasons: so that I can have a point of reference, and for this thread. Below you will find up to 100 recent biomarkers of mine.
Had to make collages because the results were scattered on the lab's platform and it took way longer than I want to admit
MAIN
High-Sensitivity C-Reactive Protein (hsCRP) 
3.48 mg/L (0-1)

C-Reactive Protein (CRP)
3.2 mg/L

Erytrocyte Sedimentation Rate (ESR)
9 mm/h (0-15)


3.48 mg/L (0-1)
C-Reactive Protein (CRP)
3.2 mg/L
Erytrocyte Sedimentation Rate (ESR)
9 mm/h (0-15)
CBC
Click the image to expand, otherwise see the list below


White Blood Cell Count (WBC)
8.38 mii/μL [4-10]
Red Blood Cell Count (RBC)
5.18 mil./μL [4.3-5.7]
Hemoglobin (Hb)
15.7 g/dL [13.2-17.3]
Hematocrit (Ht)
46.6% [39-49]
Mean Corpuscular Volume (MCV)
90fL [80-99]
Mean Corpuscular Hemoglobin (MCH)
30.3 pg/cell [27-34]
Mean Corpuscular Hemoglobin Concentration (MCHC)
33.7 g/dL [32–37]
Red Cell Distribution Width (RDW)
12.1 % [11.6–14.8]
Platelet Count
248 mii/µL [150–450]
Mean Platelet Volume (MPV)
9.7 fL [5–13]
Platelet Distribution Width (PDW)
10.9 fL [8–22.2]
Neutrophil %
63.2 % [45–80]
Neutrophil Count
5.29 mii/µL [2–8]
Lymphocyte %
26 % [20–55]
Lymphocyte Count
2.18 mii/µL [1–4]
Monocyte %
7.3 % [0–15]
Monocyte Count
0.61 mii/µL [0.3–1.0]
Eosinophil %
2.7 % [0–7]
Eosinophil Count
0.23 mii/µL [0.05–0.70]
Basophil %
0.8 % [0–2]
Basophil Count
0.07 mii/µL [0-0.2]
8.38 mii/μL [4-10]
Red Blood Cell Count (RBC)
5.18 mil./μL [4.3-5.7]
Hemoglobin (Hb)
15.7 g/dL [13.2-17.3]
Hematocrit (Ht)
46.6% [39-49]
Mean Corpuscular Volume (MCV)
90fL [80-99]
Mean Corpuscular Hemoglobin (MCH)
30.3 pg/cell [27-34]
Mean Corpuscular Hemoglobin Concentration (MCHC)
33.7 g/dL [32–37]
Red Cell Distribution Width (RDW)
12.1 % [11.6–14.8]
Platelet Count
248 mii/µL [150–450]
Mean Platelet Volume (MPV)
9.7 fL [5–13]
Platelet Distribution Width (PDW)
10.9 fL [8–22.2]
Neutrophil %
63.2 % [45–80]
Neutrophil Count
5.29 mii/µL [2–8]
Lymphocyte %
26 % [20–55]
Lymphocyte Count
2.18 mii/µL [1–4]
Monocyte %
7.3 % [0–15]
Monocyte Count
0.61 mii/µL [0.3–1.0]
Eosinophil %
2.7 % [0–7]
Eosinophil Count
0.23 mii/µL [0.05–0.70]
Basophil %
0.8 % [0–2]
Basophil Count
0.07 mii/µL [0-0.2]
IMMUNOLOGY
Click the image to expand, otherwise see the list below


Antinuclear Antibodies (ANA)
(immunofluorescence)
<1:80
Cyclic Citrullinated Peptide Antibodies (CCP)
1.3 U/mL [0–7]
Rheumatoid Factor
7 U/mL [0–14]
Immunoglobulin G (IgG)
938 mg/dL [700–1600]
Immunoglobulin M (IgM)
16.3 U/mL [0–100]
Immunoglobulin E (IgE)
114 mg/dL [40–230]
(immunofluorescence)
<1:80
Cyclic Citrullinated Peptide Antibodies (CCP)
1.3 U/mL [0–7]
Rheumatoid Factor
7 U/mL [0–14]
Immunoglobulin G (IgG)
938 mg/dL [700–1600]
Immunoglobulin M (IgM)
16.3 U/mL [0–100]
Immunoglobulin E (IgE)
114 mg/dL [40–230]
PROTEINS + SPEP
Click the image to expand, otherwise see the list below


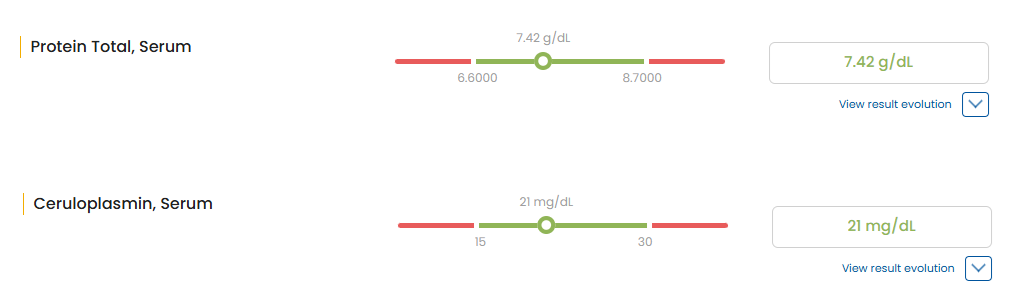
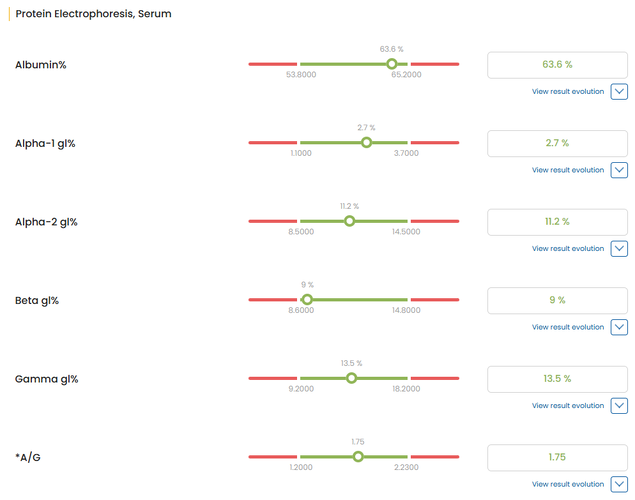
Protein Total, Serum
7.42 g/dL [6.6–8.7]
Ceruloplasmin, Serum
21 mg/dL [15–30]
Albumin %
63.6 % [53.8–65.2]
Alpha-1 globulin %
2.7 % [1.1–3.7]
Alpha-2 globulin %
11.2 % [8.5–14.5]
Beta globulin %
9.0 % [8.6–14.8]
Gamma globulin %
13.5 % [9.2–18.2]
Albumin/Globulin Ratio (A/G)
1.75 [1.20–2.23]
7.42 g/dL [6.6–8.7]
Ceruloplasmin, Serum
21 mg/dL [15–30]
Albumin %
63.6 % [53.8–65.2]
Alpha-1 globulin %
2.7 % [1.1–3.7]
Alpha-2 globulin %
11.2 % [8.5–14.5]
Beta globulin %
9.0 % [8.6–14.8]
Gamma globulin %
13.5 % [9.2–18.2]
Albumin/Globulin Ratio (A/G)
1.75 [1.20–2.23]
IRON
LIVER + BILIARY
Click the image to expand, otherwise see the list below

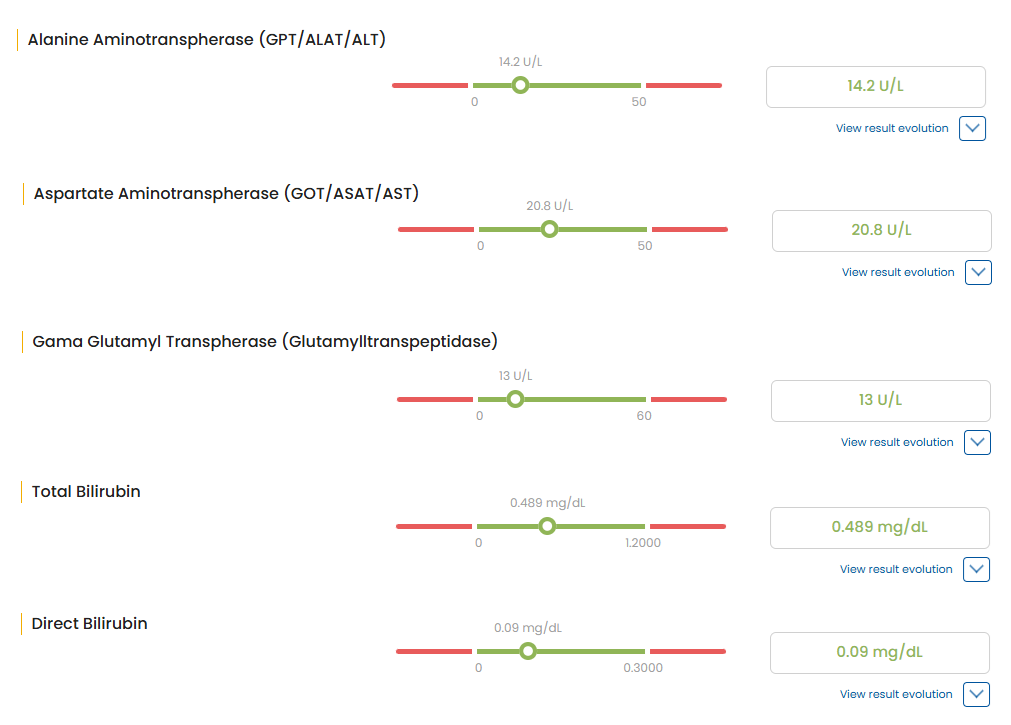
Alanine aminotransferase (ALT)
14.2 U/L [0–50]
Aspartate aminotransferase (AST)
20.8 U/L [0–50]
GGT (Gamma-glutamyl transferase)
13 U/L [0–60]
Total Bilirubin
0.489 mg/dL [0.0–1.2]
Direct Bilirubin
0.09 mg/dL [0.0–0.3]
14.2 U/L [0–50]
Aspartate aminotransferase (AST)
20.8 U/L [0–50]
GGT (Gamma-glutamyl transferase)
13 U/L [0–60]
Total Bilirubin
0.489 mg/dL [0.0–1.2]
Direct Bilirubin
0.09 mg/dL [0.0–0.3]
KIDNEY
Click the image to expand, otherwise see the list below

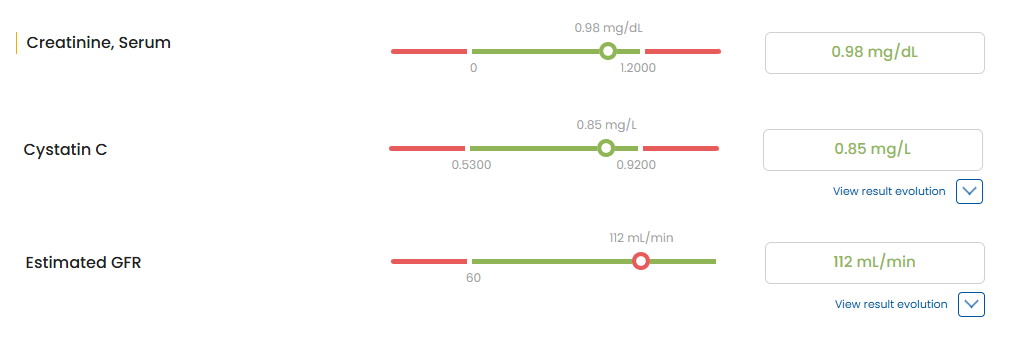
Creatinine, Serum
0.98 mg/dL [0.0–1.2]
Cystatin C
0.85 mg/L [0.53–0.92]
Estimated GFR (eGFR)
112 mL/min [≥60]
0.98 mg/dL [0.0–1.2]
Cystatin C
0.85 mg/L [0.53–0.92]
Estimated GFR (eGFR)
112 mL/min [≥60]
ELECTROLYTES + MINERALS
THYROID
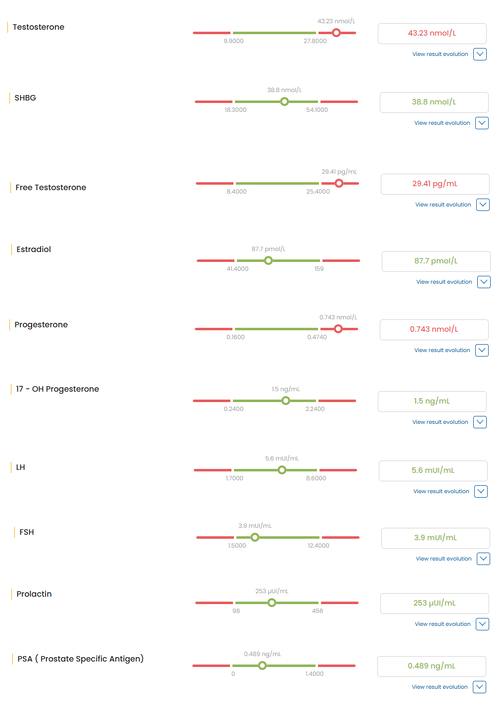
HORMONES/ENDOCRINE
Click the image to expand, otherwise see the list below



 Adrenal / pituitary / stress
Adrenal / pituitary / stress
 Gonadal / sex hormones
Gonadal / sex hormones
 Catecholamines
Catecholamines
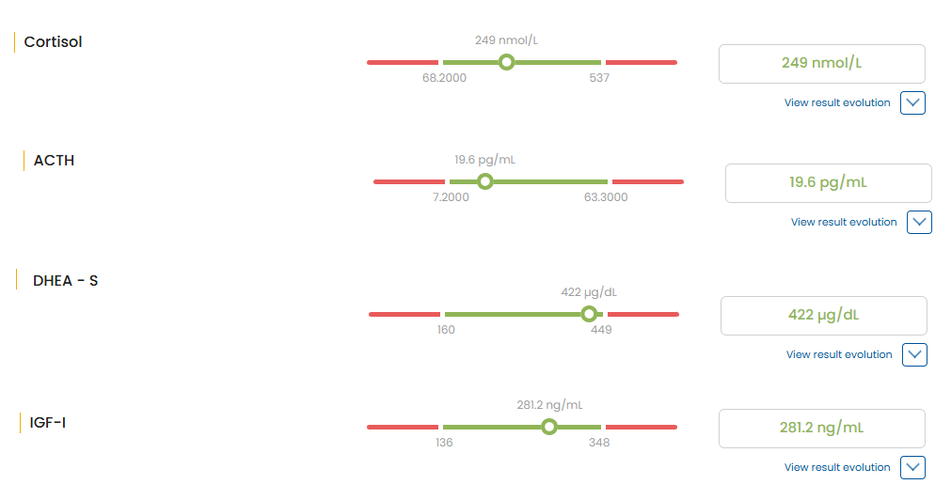
 Adrenal / pituitary / stress
Adrenal / pituitary / stressCortisol
249 nmol/L [68.2–537]
Adrenocorticotropic Hormone (ACTH)
19.6 pg/mL [7.2–63.3]
Dehydroepiandrosterone SUlfate (DHEA-S)
422 µg/dL [160–449]
Insulin-Like Growth Factor 1 (IGF-1) (Somatomedin C)
281.2 ng/mL [136–348]
249 nmol/L [68.2–537]
Adrenocorticotropic Hormone (ACTH)
19.6 pg/mL [7.2–63.3]
Dehydroepiandrosterone SUlfate (DHEA-S)
422 µg/dL [160–449]
Insulin-Like Growth Factor 1 (IGF-1) (Somatomedin C)
281.2 ng/mL [136–348]
 Gonadal / sex hormones
Gonadal / sex hormonesTestosterone (total)
43.23 nmol/L [9.9–27.8]
Free Testosterone
29.41 pg/mL [8.4–25.4]
Estradiol
87.7 pmol/L [41.4–159]
Progesterone
0.743 nmol/L [0.16–0.474]
17-Hydroxyprogesterone (17-OH Progesterone)
1.5 ng/mL [0.24–2.24]
Sex Hormone-Binding Globulin (SHBG)
38.8 nmol/L [18.3–54.1]
Prolactin
253 µIU/mL [98–456]
Luteinizing Hormone (LH)
5.6 mIU/mL [1.7–8.6]
Follicle-Stimulating Hormone (FSH)
3.9 mIU/mL [1.5–12.4]
Prostate-Specific Antigen (PSA)
0.489 ng/mL [0–1.4]
43.23 nmol/L [9.9–27.8]
Free Testosterone
29.41 pg/mL [8.4–25.4]
Estradiol
87.7 pmol/L [41.4–159]
Progesterone
0.743 nmol/L [0.16–0.474]
17-Hydroxyprogesterone (17-OH Progesterone)
1.5 ng/mL [0.24–2.24]
Sex Hormone-Binding Globulin (SHBG)
38.8 nmol/L [18.3–54.1]
Prolactin
253 µIU/mL [98–456]
Luteinizing Hormone (LH)
5.6 mIU/mL [1.7–8.6]
Follicle-Stimulating Hormone (FSH)
3.9 mIU/mL [1.5–12.4]
Prostate-Specific Antigen (PSA)
0.489 ng/mL [0–1.4]
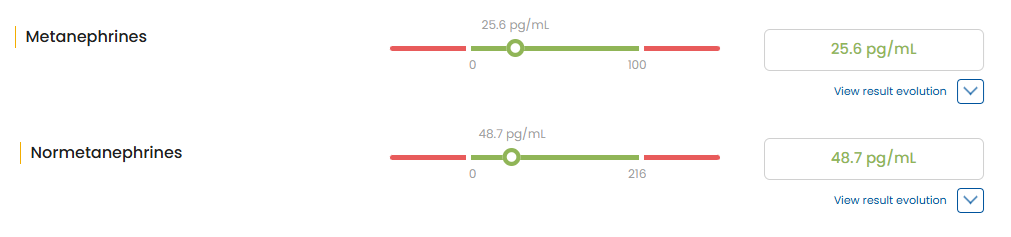
 Catecholamines
CatecholaminesMetanephrines
25.6 pg/mL [0–100]
Normetanephrines
48.7 pg/mL [0–216]
25.6 pg/mL [0–100]
Normetanephrines
48.7 pg/mL [0–216]
LIPIDS / CARDIOVASCULAR
Click the image to expand, otherwise see the list below

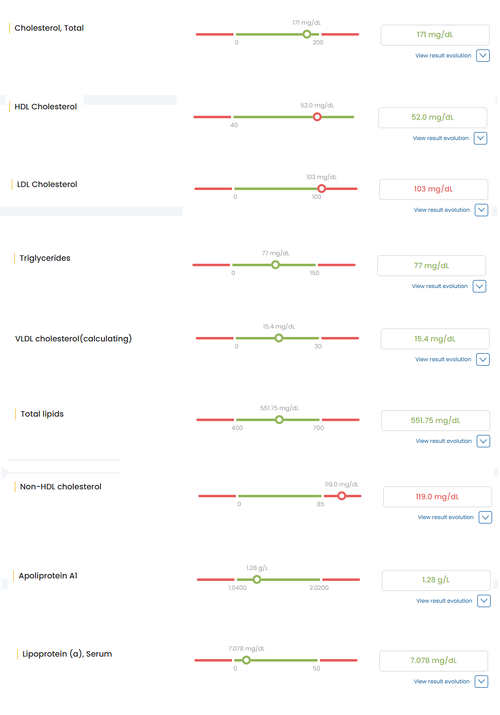
Cholesterol, Total
171 mg/dL [0–200]
HDL Cholesterol
52.0 mg/dL [40+]
LDL Cholesterol
103 mg/dL [0–100]
Triglycerides
77 mg/dL [0–150]
VLDL Cholesterol
15.4 mg/dL [0–30]
Non-HDL Cholesterol
119 mg/dL [0–85]
Total lipids
551.75 mg/dL [400–700]
Apolipoprotein A1
1.28 g/L [1.04–2.02]
Lipoprotein(a)
7.08 mg/dL [0–50]
171 mg/dL [0–200]
HDL Cholesterol
52.0 mg/dL [40+]
LDL Cholesterol
103 mg/dL [0–100]
Triglycerides
77 mg/dL [0–150]
VLDL Cholesterol
15.4 mg/dL [0–30]
Non-HDL Cholesterol
119 mg/dL [0–85]
Total lipids
551.75 mg/dL [400–700]
Apolipoprotein A1
1.28 g/L [1.04–2.02]
Lipoprotein(a)
7.08 mg/dL [0–50]
GLUCOSE / INSULIN
VITAMINS / OTHERS
Click the image to expand, otherwise see the list below


Lactate Dehydrogenase (LDH)
191 U/L [135–225]
Uric Acid, Serum
4.59 mg/dL [0–7.0]
25-OH Vitamin D
35.2 ng/mL [30–55.5]
Homocysteine, Plasma
7.6 µmol/L [0–12]
Vitamin B12
1483 pg/mL [197–771]
Holotranscobalamin (active B12)
256 pmol/L [25.1–165]
Folate, Serum
7.39 ng/mL [4.6–34.8]
191 U/L [135–225]
Uric Acid, Serum
4.59 mg/dL [0–7.0]
25-OH Vitamin D
35.2 ng/mL [30–55.5]
Homocysteine, Plasma
7.6 µmol/L [0–12]
Vitamin B12
1483 pg/mL [197–771]
Holotranscobalamin (active B12)
256 pmol/L [25.1–165]
Folate, Serum
7.39 ng/mL [4.6–34.8]
Missing bloodwork
- Fibrinogen, Interleukin-6 (IL-6), ApoB, Lp-PLA2 (vascular inflammation), Oxidized LDL
- Full allergy workup
- tTG-IgA ± total IgA for Celiac serology
- Fecal calprotectin for gut inflammation/IBD (highly doubt this would be the cause)
- Full allergy workup
- tTG-IgA ± total IgA for Celiac serology
- Fecal calprotectin for gut inflammation/IBD (highly doubt this would be the cause)
TLDR
Just read the thread if you're interested.
Open to being wrong about anything, I'm just trying to make this a useful reference thread.
Any input is highly appreciated, especially corrections, causes I might've missed or your own experiences with elevated hsCRP.
Cheers,
Nexo