holy
- Joined
- Nov 5, 2024
- Posts
- 954
- Reputation
- 1,690

(catching cavities before they happen)
The information provided in this teeth guide is for general informational purposes only and is not intended as a substitute for professional dental or medical advice, diagnosis, or treatment. Always seek the advice of a qualified dentist, orthodontist, or other licensed healthcare professional with any questions you may have regarding your dental health or a specific dental condition.
TABLE OF CONTENTS:
1. Introduction
2. Fluoride (or hydroxyapatite) remineralization
3. Calcium + phosphate availability
4. Saliva flow and ph control
5. Diet control
6. Oral microbiome shift
7. Actual professional help
What do I mean "pre-cavity"? Well, it usually means demineralization of enamel, not yet a physical hole that a dentist has to drill.
Once it’s cavitated (actual hole), you can’t reverse it, you can only restore.
But pre-cavity (white spot lesion stage) can be reversed because the tooth structure is still there, just weakened.
The trick is to shift the chemistry of your mouth so minerals flow into enamel instead of out.
In this guide, I will precisely show you how that works in practice.
Once it’s cavitated (actual hole), you can’t reverse it, you can only restore.
But pre-cavity (white spot lesion stage) can be reversed because the tooth structure is still there, just weakened.
The trick is to shift the chemistry of your mouth so minerals flow into enamel instead of out.
In this guide, I will precisely show you how that works in practice.
Enamel is mostly hydroxyapatite (ca₁₀(po₄)₆(oh)₂). Acids from bacteria dissolve calcium and phosphate ions out.
Fluoride replaces the hydroxyl (oh⁻) group, forming fluorapatite (ca₁₀(po₄)₆f₂). This crystal is more stable, dissolves slower in acid, and resists further demineralization.
Fluoride also catalyzes remineralization by attracting calcium and phosphate back into enamel. It makes the rebuilding faster and stronger.
Fluoride replaces the hydroxyl (oh⁻) group, forming fluorapatite (ca₁₀(po₄)₆f₂). This crystal is more stable, dissolves slower in acid, and resists further demineralization.
Fluoride also catalyzes remineralization by attracting calcium and phosphate back into enamel. It makes the rebuilding faster and stronger.
Instead of relying on fluoride chemistry, you literally give your teeth hydroxyapatite particles.
They integrate into microscopic defects and act like a patch, filling in the softened enamel. This is basically “rebuilding with bricks” instead of just “making the wall harder.”
Multiple RCTS (randomized controlled trials) show nano-hydroxyapatite is comparable to fluoride for remineralizing early caries.
They integrate into microscopic defects and act like a patch, filling in the softened enamel. This is basically “rebuilding with bricks” instead of just “making the wall harder.”
Multiple RCTS (randomized controlled trials) show nano-hydroxyapatite is comparable to fluoride for remineralizing early caries.
1. In-situ, double-blind, crossover study (adults, enamel blocks)

- Participants wore oral appliances with enamel blocks subjected to one of three dentifrices:
5 % nHAP, 10 % nHAP, or 1100 ppm fluoride.
- Both mineral loss (ΔZ) and lesion depth were significantly reduced in all groups (p < 0.001).
Crucially, remineralization was statistically comparable across nHAP and fluoride groups
2. Triple-blind randomized clinical trial (children, 24-month follow-up)

- Enrolled 610 children (ages 4–7).
- Toothpastes: two hydroxyapatite-fluoride (HAF) variants (1000 and 1450 ppm F) vs. two mono-fluoride (NaMFP) toothpastes.
- After two years, HAF toothpaste led to a significantly greater reduction in active enamel lesions (p < .01).
Nearly three-quarters of previously active lesions in the HAF group were inactive at follow-up (p = .04 vs. NaMFP)
3. Clinical comparative study (initial carious lesions in vivo)

Ninety initial lesions randomized to:
- (A) tricalcium phosphate (TCP),
(B) fluoride varnish, and
(C) nano-hydroxyapatite gel.
All treatments were effective, but nHAP scored highest, significantly superior remineralization than both TCP and fluoride varnish (p = 0.007 vs. fluoride)
There's also lab-based and pH-cycling studies with similar conclusions but you get the point.

- Participants wore oral appliances with enamel blocks subjected to one of three dentifrices:
5 % nHAP, 10 % nHAP, or 1100 ppm fluoride.
- Both mineral loss (ΔZ) and lesion depth were significantly reduced in all groups (p < 0.001).
Crucially, remineralization was statistically comparable across nHAP and fluoride groups
2. Triple-blind randomized clinical trial (children, 24-month follow-up)
- Enrolled 610 children (ages 4–7).
- Toothpastes: two hydroxyapatite-fluoride (HAF) variants (1000 and 1450 ppm F) vs. two mono-fluoride (NaMFP) toothpastes.
- After two years, HAF toothpaste led to a significantly greater reduction in active enamel lesions (p < .01).
Nearly three-quarters of previously active lesions in the HAF group were inactive at follow-up (p = .04 vs. NaMFP)
3. Clinical comparative study (initial carious lesions in vivo)

Ninety initial lesions randomized to:
- (A) tricalcium phosphate (TCP),
(B) fluoride varnish, and
(C) nano-hydroxyapatite gel.
All treatments were effective, but nHAP scored highest, significantly superior remineralization than both TCP and fluoride varnish (p = 0.007 vs. fluoride)
There's also lab-based and pH-cycling studies with similar conclusions but you get the point.
1. Fluoride toothpaste (1350–1500 ppm fluoride):

(Picture of oral-b pro-expert toothpaste)
OR

(Picture of regular sensodyne toothpaste)
Brush gently but thoroughly, especially around those white spots.
DON'T RINSE IMMEDIATELY AFTER BRUSHING, just spit out the excess. You want that fluoride to sit on your teeth for a while.
2. High-fluoride prescription pastes (5000 ppm):

(Picture of 3M Clinpro 5000)
OR

(Pictuere of colgate duraphor toothpaste)
Dentists give these if you’re high risk. Stronger remineralization effect.
3. Fluoride mouthrinses (0.05% daily OR 0.2% weekly sodium fluoride)

(Picture of X-Pur 0.5% Fluoride Opti-Rinse)
OR

(Picture of X-Pur 0.5% Opti-Rinse)
Adds an extra layer, especially for high sugar intake.
4. Fluoride varnish/professional gels:

(Picture of FluoriMax 2.5% Sodium Fluoride Varnish)
Dentist-applied, much higher concentration, sticks to teeth for hours.
5. Hydroxyapatite toothpaste (usually 10% n-ha):

(Picture of Nano-Hydroxyapatite Toothpaste)
Same brushing method, but safe to swallow, often marketed as fluoride-free alternative.
You can, obviously, pick from any brand. It really doesn't matter. But, make sure it's from reputable brands.

(Picture of oral-b pro-expert toothpaste)
OR

(Picture of regular sensodyne toothpaste)
Brush gently but thoroughly, especially around those white spots.
DON'T RINSE IMMEDIATELY AFTER BRUSHING, just spit out the excess. You want that fluoride to sit on your teeth for a while.
2. High-fluoride prescription pastes (5000 ppm):

(Picture of 3M Clinpro 5000)
OR

(Pictuere of colgate duraphor toothpa
Dentists give these if you’re high risk. Stronger remineralization effect.
3. Fluoride mouthrinses (0.05% daily OR 0.2% weekly sodium fluoride)

(Picture of X-Pur 0.5% Fluoride Opti-Rinse)
OR

(Picture of X-Pur 0.5% Opti-Rinse)
Adds an extra layer, especially for high sugar intake.
4. Fluoride varnish/professional gels:

(Picture of FluoriMax 2.5% Sodium Fluoride Varnish)
Dentist-applied, much higher concentration, sticks to teeth for hours.
5. Hydroxyapatite toothpaste (usually 10% n-ha):

(Picture of Nano-Hydroxyapatite Toothpaste)
Same brushing method, but safe to swallow, often marketed as fluoride-free alternative.
You can, obviously, pick from any brand. It really doesn't matter. But, make sure it's from reputable brands.
You need a daily supply of fluoride or hydroxyapatite so enamel stays saturated and remineralization is always favored over demineralization.
Saliva is supersaturated with calcium and phosphate under normal ph. That’s why your teeth don’t dissolve constantly.
When ph drops below ~5.5, saturation breaks, minerals leach out. When ph rises again, saliva can redeposit them.
If saliva is low (dry mouth, dehydration, meds, mouth breathing), remineralization slows to a crawl.
When ph drops below ~5.5, saturation breaks, minerals leach out. When ph rises again, saliva can redeposit them.
If saliva is low (dry mouth, dehydration, meds, mouth breathing), remineralization slows to a crawl.
Calcium isn't just about drinking milk (though dairy helps).
- Leafy greens
- Almonds
- Sardines with bones
- Fortified plant milks
Phosphate comes from protein sources like:
- Fish
- Eggs
- Meat
If you're vegan:
- Quinoa
- Pumpkin seeds
These are decent sources.
You need vitamin D3 and vitamin K2 to actually use the calcium effectively. D3 helps you absorb calcium from your gut, k2 makes sure it goes to your teeth and bones instead of your arteries.
1. Get some sun,
2. Take a d3 supplement,
3. And eat fermented foods or take k2.
- Calcium and phosphate mouth rinses can help too. You can make your own by dissolving a pinch of calcium chloride and a smaller pinch of potassium phosphate in water, but honestly, just buy a remineralizing mouthwash.
CCPPACP (casein phosphopeptide-amorphous calcium phosphate) products work really well for this.
- Leafy greens
- Almonds
- Sardines with bones
- Fortified plant milks
Phosphate comes from protein sources like:
- Fish
- Eggs
- Meat
If you're vegan:
- Quinoa
- Pumpkin seeds
These are decent sources.
You need vitamin D3 and vitamin K2 to actually use the calcium effectively. D3 helps you absorb calcium from your gut, k2 makes sure it goes to your teeth and bones instead of your arteries.
1. Get some sun,
2. Take a d3 supplement,
3. And eat fermented foods or take k2.
- Calcium and phosphate mouth rinses can help too. You can make your own by dissolving a pinch of calcium chloride and a smaller pinch of potassium phosphate in water, but honestly, just buy a remineralizing mouthwash.
CCPPACP (casein phosphopeptide-amorphous calcium phosphate) products work really well for this.
Saliva is your body’s natural buffer. It keeps ph around neutral (6.7–7.4).
It carries calcium, phosphate, and proteins that coat enamel and prevent dissolution.
It literally washes away acids and food particles. Without enough saliva, even the best toothpaste is crippled.
It carries calcium, phosphate, and proteins that coat enamel and prevent dissolution.
It literally washes away acids and food particles. Without enough saliva, even the best toothpaste is crippled.
Bacteria ferment sugar, producing lactic acid. Enamel starts dissolving below ph 5.5.
The longer ph stays low, the more minerals leach out.
When ph bounces back above 5.5, saliva can redeposit minerals.
The longer ph stays low, the more minerals leach out.
When ph bounces back above 5.5, saliva can redeposit minerals.
1. Chew sugar-free gum after meals, especially gum with xylitol. The chewing stimulates saliva production, and xylitol actually starves the harmful bacteria in your mouth. 6-10 grams of xylitol daily, spread throughout the day.
2. Drink more water, but not just any water. If your tap water has fluoride, great. If not, consider fluoridated or remineralizing water.
"Muh, fluoride water bad!"
Usually comes from people who haven’t actually looked at the data.
At the concentrations used in municipal water (typically 0.7 mg/L in the us, similar in other countries), it prevents tooth decay without meaningful systemic harm.
At toxic levels, sure, fluoride can cause dental or skeletal fluorosis. But that’s not what’s happening in regulated water supplies.
It’s the same logic as saying “salt is bad because if you eat 3 cups of it you’ll die.”
No one is dosing their water with 3 cups of salt.
3. Avoid constantly sipping acidic drinks like coffee, tea, or anything with lemon. If you do drink them, always rinse with water afterward.
4. Don’t brush immediately after acidic drinks (like soda or citrus). The enamel surface is softened, and brushing scrapes it. Wait 30 minutes for saliva to re-harden it.
5. Give saliva 2–3 hours between meals for remineralization to actually happen.
5. Test your saliva ph with strips if you're really serious about this. Healthy saliva should be around 6.5-7.5. If yours is consistently acidic, you might need to look at your diet, stress levels, or medications that could be affecting it.
2. Drink more water, but not just any water. If your tap water has fluoride, great. If not, consider fluoridated or remineralizing water.
"Muh, fluoride water bad!"
Usually comes from people who haven’t actually looked at the data.
At the concentrations used in municipal water (typically 0.7 mg/L in the us, similar in other countries), it prevents tooth decay without meaningful systemic harm.
At toxic levels, sure, fluoride can cause dental or skeletal fluorosis. But that’s not what’s happening in regulated water supplies.
It’s the same logic as saying “salt is bad because if you eat 3 cups of it you’ll die.”
No one is dosing their water with 3 cups of salt.
3. Avoid constantly sipping acidic drinks like coffee, tea, or anything with lemon. If you do drink them, always rinse with water afterward.
4. Don’t brush immediately after acidic drinks (like soda or citrus). The enamel surface is softened, and brushing scrapes it. Wait 30 minutes for saliva to re-harden it.
5. Give saliva 2–3 hours between meals for remineralization to actually happen.
5. Test your saliva ph with strips if you're really serious about this. Healthy saliva should be around 6.5-7.5. If yours is consistently acidic, you might need to look at your diet, stress levels, or medications that could be affecting it.
Dentists can measure salivary flow rate and buffer capacity. People with dry mouth (xerostomia) are at extreme risk for cavities even if they brush well, simply because the buffering system is gone.
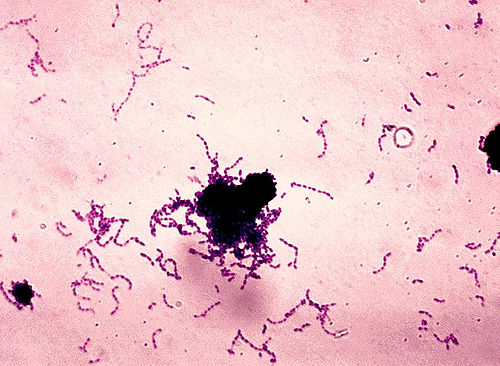
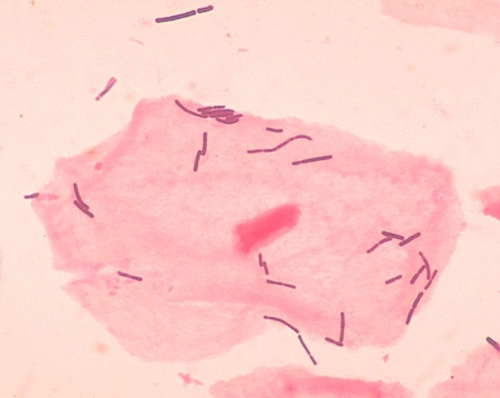
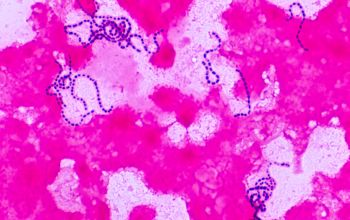
Cavity bacteria:

(s. mutans)

(lactobacilli)
These ferment fermentable carbs (sucrose, glucose, fructose, cooked starches).
The byproduct is acid. Enamel dissolves once ph dips below 5.5.
Every “sugar hit” = ~20–40 minutes of acidic conditions. If you keep snacking, ph never recovers, remineralization stalls, and net mineral loss happens.
(s. mutans)
(lactobacilli)
These ferment fermentable carbs (sucrose, glucose, fructose, cooked starches).
The byproduct is acid. Enamel dissolves once ph dips below 5.5.
Every “sugar hit” = ~20–40 minutes of acidic conditions. If you keep snacking, ph never recovers, remineralization stalls, and net mineral loss happens.
Eating 50 g sugar in one sitting is less harmful than sipping 10 g sugar every 30 minutes across the day. The first gives one long acid attack, the second keeps teeth under constant assault.
This is why “grazing” and sipping sodas/juices is so destructive.
This is why “grazing” and sipping sodas/juices is so destructive.
1. If you’re going to have sweets, do it with meals, not between them. Meals stimulate saliva flow and help neutralize acids faster.
2. Things like raisins, gummies, or bread paste into fissures and hold sugar against enamel longer than chocolate or ice cream (which wash away faster).
3. Use xylitol as a sugar substitute. Bacteria can’t metabolize it, so no acid production. It also shifts the oral microbiome toward less cariogenic species.
5. Drink water after sugar. This dilutes acids and helps saliva restore ph.
6. Cheese, milk, yogurt have calcium, phosphate, and casein are all protective. They buffer acid and promote remineralization.
7. Limit energy drinks, soda, fruit juice. They combine direct acid erosion with sugar fermentation. If you drink them, do it with meals and use a straw to minimize enamel contact.
2. Things like raisins, gummies, or bread paste into fissures and hold sugar against enamel longer than chocolate or ice cream (which wash away faster).
3. Use xylitol as a sugar substitute. Bacteria can’t metabolize it, so no acid production. It also shifts the oral microbiome toward less cariogenic species.
5. Drink water after sugar. This dilutes acids and helps saliva restore ph.
6. Cheese, milk, yogurt have calcium, phosphate, and casein are all protective. They buffer acid and promote remineralization.
7. Limit energy drinks, soda, fruit juice. They combine direct acid erosion with sugar fermentation. If you drink them, do it with meals and use a straw to minimize enamel contact.
If it spends more time below, cavities progress. If more time above, remineralization wins.
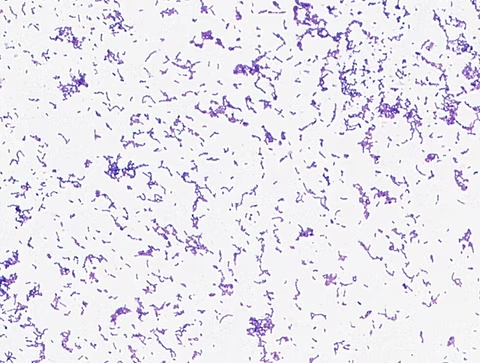
Streptococcus mutans: Primary acid producer in early cavities. thrives on sugar, sticks to enamel, forms sticky biofilm.
Lactobacilli: Secondary acid producers, favor deeper lesions.
“Good” bacteria:
1. Streptococcus sanguinis

2. Streptococcus gordonii,

3. and others that produce less acid and compete with the bad ones
Lactobacilli: Secondary acid producers, favor deeper lesions.
“Good” bacteria:
1. Streptococcus sanguinis
2. Streptococcus gordonii,
3. and others that produce less acid and compete with the bad ones
1. Xylitol is your best friend here. It literally starves the bad bacteria because they can't digest it, but they keep trying until they die. Meanwhile, beneficial bacteria can handle xylitol just fine.
2. Probiotic toothpastes and mouth rinses are becoming more common. Look for products with streptococcus salivarius k12 or lactobacillus reuteri. These beneficial bacteria can help crowd out the bad bacteria.
3. Oil pulling with coconut oil might help too. Swish a tablespoon around for 10-15 minutes (work up to this gradually), then spit it out. The lauric acid in coconut oil has antimicrobial properties that seem to target harmful bacteria more than beneficial ones.
2. Probiotic toothpastes and mouth rinses are becoming more common. Look for products with streptococcus salivarius k12 or lactobacillus reuteri. These beneficial bacteria can help crowd out the bad bacteria.
3. Oil pulling with coconut oil might help too. Swish a tablespoon around for 10-15 minutes (work up to this gradually), then spit it out. The lauric acid in coconut oil has antimicrobial properties that seem to target harmful bacteria more than beneficial ones.
If you're seeing white spots, get them professionally evaluated. Your dentist can confirm they're early decay and not something else like fluorosis or enamel hypoplasia. They can also apply professional-strength fluoride treatments that work faster than anything you can do at home.
Professional remineralization treatments use higher concentrations of fluoride, calcium, and phosphate than over-the-counter products. Some dentists offer cppacp applications or even newer treatments like silver diamine fluoride for arrested decay
Regular cleanings become more important when you're trying to reverse early decay. Professional cleaning removes the biofilm that protects harmful bacteria and allows remineralizing agents to reach the tooth surface better.
Your dentist might recommend:
1. prescription-strength fluoride toothpaste
OR
2. custom remineralization protocols
This is based on your specific situation.
They can also help identify and fix factors that are contributing to the problem, like dry mouth from medications or grinding that's wearing away enamel.
Professional remineralization treatments use higher concentrations of fluoride, calcium, and phosphate than over-the-counter products. Some dentists offer cppacp applications or even newer treatments like silver diamine fluoride for arrested decay
Regular cleanings become more important when you're trying to reverse early decay. Professional cleaning removes the biofilm that protects harmful bacteria and allows remineralizing agents to reach the tooth surface better.
Your dentist might recommend:
1. prescription-strength fluoride toothpaste
OR
2. custom remineralization protocols
This is based on your specific situation.
They can also help identify and fix factors that are contributing to the problem, like dry mouth from medications or grinding that's wearing away enamel.
These cover the full spectrum of early cavity reversal, from fluoride and hydroxyapatite to saliva, diet, microbiome balance, and professional interventions:
1.
[Cavity formation mechanics and emphasizes maintaining an alkaline oral environment, which naturally ties into saliva function, diet control, and remineralization strategies]
2.
[Walks through how early cavities can be reversed and how to prevent future ones]
3.
[Breaks down techniques to remineralize teeth and prevent decay, touching on multiple pillars like fluoride use, diet, and oral hygiene]
1.
[Cavity formation mechanics and emphasizes maintaining an alkaline oral environment, which naturally ties into saliva function, diet control, and remineralization strategies]
2.
[Walks through how early cavities can be reversed and how to prevent future ones]
3.
[Breaks down techniques to remineralize teeth and prevent decay, touching on multiple pillars like fluoride use, diet, and oral hygiene]




